In the Direct Acting Antiviral (DAA) era, treatments for hepatitis C virus (HCV) are easier to take, with fewer side effects, and for a shorter duration, yet the high cost of drugs and insurance companies’ unwillingness to pay for treatment keeps the hope of cure out of reach for most living with HCV. This article explores the many benefits of curing HCV, and makes a case that people living with this disease should reap the benefits of cure.
Hepatitis C virus (HCV) is chronic progressive liver disease.
TO BE MORE PRECISE, HCV is chronic progressive liver disease that can be cured.
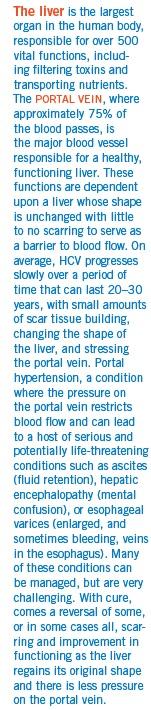
Without a cure, up to 20% of people with HCV will develop cirrhosis (scarring that damages the liver, causing it to not function properly) in 20–30 years. There are several additional factors, such as alcohol consumption or HIV/HCV co-infection, that can both increase the risk of developing, and speed up this rate of, cirrhosis. Among those patients with cirrhosis, there is a 1–5% annual risk of developing liver cancer, and a 3–6% annual risk of hepatic decompensation (disease progression requiring a liver transplant). Once people are diagnosed with a decompensated liver, their risk of death in the next year runs between 15–20%.1
Early treatment and cure of hepatitis C can virtually eliminate all of these long-term complications.
Although a minority opinion, it has been argued that not everyone progresses to cirrhosis and end-stage liver disease, making HCV treatment and cure not valuable or cost effective.2 Tell that to a person who is infected with HCV and lives with the daily stress that comes from living with a chronic disease and the uncertainty of knowing if they will be one of those who will develop cirrhosis. Tell that to the woman of child-bearing age who would like to treated and cured before becoming pregnant and starting a family. Tell that to a person who does not want to transmit HCV to their sexual or drug-using partner.
People with HCV want to be cured, and we have effective treatments that can cure them. And yet, we have large numbers of patients who cannot access HCV treatment due to the refusal of insurance companies or Medicaid programs to pay for them for a variety of reasons including, but not limited to, active or recent substance use, livers that are deemed too healthy, or restrictions on the number of times a person can be treated. None of these excuses are based on clinical evidence or public health concerns, and expert medical opinion calls for the treatment of all people with HCV.3
Even before the DAA era, we had evidence of the benefits that come from curing HCV.4 Today, we are now seeing more and more people cured of HCV. With this comes increased knowledge about the clinical value of a cure, as well as the more subjective improved quality of life experienced by those who are cured. Consequently, there has been a flood of research that demonstrates the benefits of an HCV cure for the individual, the public health, and society.
What is an HCV cure?
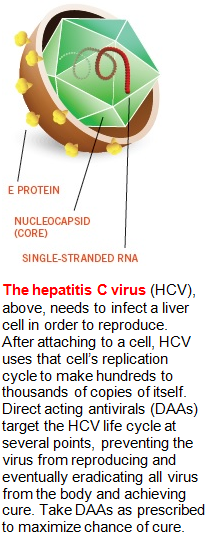
The term sustained virologic response, or SVR, is used to describe a cure for HCV. When HCV treatment is successful, a person will have an undetectable HCV viral load. This person is followed for 12 weeks (with periodic viral load tests to look for a return of the virus). If a person has no virus and remains undetectable after 12 weeks, they achieve an SVR12, which is considered a virologic cure—and in most cases they will remain undetectable after they finish their treatment.
The term “undetectable” can sometimes lead to confusion. Patients will often ask: Does this mean the virus is completely gone? The answer is yes. HCV is no longer found in the blood or in the liver. A patient could not undergo an HCV genotype test because there is no virus to test. The virus is gone.
But is the cure permanent? HCV recurrence after 12 weeks of SVR is extremely rare: Less than 1% of cured patients experience a late relapse.5
People who have been cured of hepatitis C will always test positive for HCV antibodies, but they no longer have virus in their body doing damage to their liver, nor do they have any virus to infect others. If a person is exposed to HCV at a later date, re-infection can happen, making prevention health education and the provision of tools such as clean syringes and other injecting supplies, and improved access to substance use and behavioral health services, an extremely important part of any HCV treatment program. But an SVR is a cure, and the liver starts to heal and function better once the virus is gone.
Personal benefits of a cure
To the person living with HCV, the benefits of getting cured are many. It is worth noting that these benefits are found not only in HCV mono-infected persons, but also people living with HIV/HCV co-infection and in people following a liver transplant.
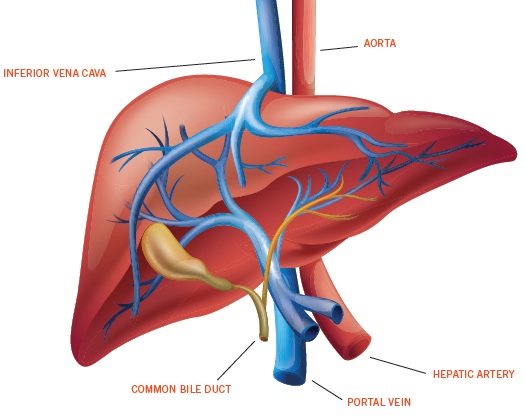
Once cure is achieved, most people experience an improvement in liver functioning, and many experience a reversal of fibrosis (mild scarring) over time. Even patients who have cirrhosis (severe scarring) experience improved liver function and a reduction in the risk of developing end-stage liver complications. There is evidence that even cirrhosis can be reversed once SVR is achieved. In reviews that have looked at changes in the liver over time, the shape of the liver can slowly return to normal, as do many of its functions. Liver enzymes improve, as do platelet counts of cured patients.6
This reduction in fibrosis and return to normal liver function comes with a host of other longer-term benefits, not the least of which is extension of life. Cured patients live longer than people who are not. A cure improves the life expectancy of people with HCV, including those with cirrhosis.
With cure from HCV comes a clinical improvement in a variety of medical conditions that occur outside the liver (extrahepatic). Conditions such as cryoglobulinemia or porphyria cutenea tarda clinically improve, or in some cases disappear. Curing HCV also reduces the risk of developing diabetes.
In addition to the clinical benefits of HCV cure, there is an additional body of literature that looks at the more subjective, personal experience, called “patient-reported outcomes” (PROs). PROs are measurements about a person’s health and well-being that come from a survey or questionnaire that comes directly from the patient.7 Reviews of PROs for people with HCV show that with cure comes reduction in fatigue, depression, insomnia, and chronic pain. People report reductions in anxiety and worry. In every aspect of quality of life, people cured of HCV report improvements. As one patient stated, “I had no idea how sick I was until I got cured of HCV.”
Public health and societal benefits of a cure
For all the personal benefits of cure, there are societal benefits, too. Both in terms of public health (reduced HCV transmission) and cost-effectiveness (utilization of fewer health resources and increased productivity in the workforce), the benefits run deep.
As with HIV, HCV treatment and reducing viral load to undetectable levels can dramatically reduce the risk of transmitting the virus to others. With HCV cure, there is no virus left, so the risk of transmission is not only reduced, it’s eliminated: A cured patient cannot transmit HCV to anyone else. In a model looking at the impact of increased screening and treatment in a variety of countries, researchers found that even a small increase in HCV screening and treatment can have an enormous impact on the burden of HCV. A treatment rate of 10% could lead to near-elimination of HCV overall.8
HCV TREATMENT AND CURE PUTS AN END TO THE
DOWNWARD SPIRAL OF DIMINISHING PRODUCTIVITY.
Treatment, or cure as prevention, can have an even greater impact on populations that are most affected by HCV, such as people who inject drugs (PWIDs) and HIV-positive MSM (men who have sex with men) at risk of sexual transmission. In a mathematical model looking at the prevention impact that comes from treating PWIDs, HCV prevention expert Natasha Martin, PhD, found that even if a small number of PWIDs were treated, there would be a 25% reduction in HCV in this population, and this benefit increases the more treatment that is provided.9 Although we do not have models or research studies assessing the impact of HCV cure as prevention in HIV/HCV co-infected persons at risk through sexual transmission, a prediction would seem to follow logically that routine HCV screening and treatment of patients who are co-infected with HIV would lead to similar reductions of new infections.
Cost effectiveness of HCV treatment
In spite of studies that have demonstrated the cost-effectiveness of these new HCV treatments, the dominant narrative in the media and policy discussions revolve around the high cost. As Dr. John Bartlett stated, “What does it mean when a drug can be cost effective, but no one can afford to take it?”
There has been much research on the cost-effectiveness of HCV treatment. Cost effectiveness is a complex subject. It is a mathematical model that looks at both the quantity (how long one lives with or without treatment), and the quality of life (either with or without treatment), accounting for the burden of disease that comes with living with symptoms such as fatigue or chronic pain.
In a sweeping review of both the clinical and financial value of HCV treatments, the California Technology Assessment Forum (CTAF) found that while treating all patients regardless of liver disease severity was expensive, it met the benchmark for cost-effectiveness in terms of the benefits gained.10
A number of other cost effectiveness studies have found similar results, with the economic benefits increasing as the cost of HCV medications go down.11
All cost effectiveness studies find that waiting to treat for more advanced liver disease significantly increases cost, and Dr. Sammy Saab and colleagues have shown that the cost per cure is lower for both treatment-naïve and non-cirrhotic patients, providing further evidence for the effectiveness of an early HCV treatment strategy.12
This strategy was further strengthened by a review of HCV treatments, where researchers found it to be a cost-effective option for patients across the spectrum of liver disease, with both short- and long-term health and economic benefits.13
Another area of HCV that has received little attention, but has significant benefits to both individuals and society, is worker productivity. It has been found that people with HCV miss more days from work, and are less productive when at work, primarily due to HCV-associated fatigue. The effect gets worse as HCV disease progresses and liver function worsens.
Further, this has a domino-like effect, as decreased worker productivity also affects the HCV patient’s caregiver, often a partner or family member, whose productivity also worsens as they miss work to take care of their loved one.
HCV treatment and cure puts an end to the downward spiral of diminishing productivity. Recent research indicates that people are able to work while on DAAs, and once cure is achieved, their absenteeism is reduced and their productivity increases dramatically.14
Treating and curing HCV lowers healthcare costs for all patients, including those with end-stage liver disease. In a review of 33,309 patients with HCV, 4,111 of whom received treatment, it was found that those who were treated and cured of HCV had significantly lower medical expenses than those who were not.14 These savings increased as the severity of HCV disease increased. The average monthly healthcare costs of those with no or little fibrosis was $885 for the treated group and $1,370 in the untreated, while those with cirrhosis had costs of $1,369 (treated) versus $1,802 (untreated). Lastly, the costs of treated versus untreated patients in end-stage liver disease saw a significant increase in monthly cost of $3,547 and $5,137 respectively.15 Other studies have come to similar findings and have highlighted the long-term cost savings associated with curing HCV, further cementing the rationale for treating all people with HCV.
In short: Treating people now saves money later
Conclusions
The benefits of curing HCV far outweigh the costs. The high cost of HCV drugs is often cited as a reason to defer or refuse treatment, a rationale that does not hold up to the scrutiny of cost effectiveness analyses. That said, regardless of affordability, these drugs have value. They cure people, extend life, eliminate risk of transmission, reduce suffering, and save money in the long run while improving worker productivity. They should be available to all people living with HCV.
THERE IS NO CLINICAL REASON TO MAKE A BLANKET DENIAL OF TREATMENT
BASED SOLELY ON A PERSON’S CURRENT OR PAST SUBSTANCE USE.
TREATING PEOPLE WHO USE DRUGS
IN 2001, Brian Edlin and colleagues wrote an opinion piece in the New England Journal of Medicine titled, “Is it justifiable to withhold treatment for hepatitis C from illicit drug users?”1 At the time, withholding treatment was indeed the standard set by the National Institutes of Health (NIH) in a consensus statement on managing HCV, which called for at least six months of abstinence from alcohol or drugs before initiating treatment. Back then, HCV treatment consisted of 6–12 months of interferon and ribavirin, and was extremely difficult to take. It is true that some people who used drugs were not able to successfully complete treatment. It’s equally true people who did not use drugs were not able to complete treatment. Whether one used drugs or not, these medications were hard to take.
Regardless, the NIH recommendations served as a barrier to care and treatment of people who used drugs. Edlin and his co-authors identified four reasons used to withhold HCV treatment in people who use drugs (PWUDs)—poor adherence to treatment, inability to cope with side effects, high risk of reinfection with HCV following cure, and the lack of urgency to start treatment overall—and they provided evidence to refute these assumptions and recommendations to overcome them. This influential article helped change these recommendations so that by the end of 2002, the NIH consensus statement was changed to allow for treatment decisions for people who use drugs to be made on a case-by-case basis.
The stigma of drug use and the belief that drug users could not be treated remained, however, and many providers held onto the earlier recommendations, and refused to treat patients who were using substances. Similarly, patients who used drugs would self-select and not seek treatment, assuming that they would not get it.
Fast forward to 2015, and much has changed in the treatment world. These changes eliminate many of the earlier arguments for denying treatment to PWUDs. As stated earlier, shorter durations, simplified regimens with no interferon injections, and minimal side effects have simplified treatment and improved adherence. Re-infection is still possible, and studies have demonstrated that it does happen, but at low rates—0.8 to 4.7 per 100 person years.2 Further, with a robust harm reduction program of clean syringes and injection supplies, access to drug treatment and opiate-substitution (methadone or buprenorphone) therapy and other prevention interventions, re-infection can be reduced further. The ease of treatment and benefits that come with cure can and should be available to all people who have HCV, including those who use drugs. Yet it is not.
The lack of urgency to treat PWUDs remains, as does the stigma and discrimination toward PWUDs.
That said, we know that PWUDs can and have been treated and cured. Even in days of pegylated interferon and ribavirin, adherence rates and treatment outcomes were similar to those of their non-drug using counterparts. With newer treatments, there is no clinical reason to make a blanket denial of treatment based solely on a person’s current or past substance use. The treatments work in the same way and cure at the same rates among PWUDs as they do in those who do not use substances. Treatment decisions should be made on a case by case basis between the patient and medical provider. In some cases, extra support around medication adherence, mental health issues, and other medical aspects of managing HCV may be needed, but these are problems that may affect non-drug users as well and are not unique to PWUDs. Drug use alone should not be a discriminatory factor in preventing cure. Indeed, as we will see in the accompanying article, treating and curing PWUDs has larger public health implications, as it will reduce or eliminate new infections.
As the AASLD/IDSA/IAS-USA HCV Guidelines state, “Recent and active injection drug use should not be seen as an absolute contraindication to HCV therapy. Scale up of HCV treatment in persons who inject drugs is necessary to positively impact the HCV epidemic in the United States and globally.”3
—ANDREW REYNOLDS
ANDREW REYNOLDS is the Hepatitis C Education Manager at Project Inform, and facilitates several HCV support groups in the San Francisco Bay Area. He’s also a counselor on the HELP-4-HEP HCV phoneline listed in the resources section of this issue. Call him if you have any questions about HCV care and treatment.