“I love what I do; it’s crazy as hell. All my family and friends are like, Aaahhh, we don’t know what she does.”
She is Neva Chauppette, PsyD, a licensed psychologist in California, and what she’s done is treat over 1,500 patients with HIV who have multiple co-occurring conditions such as addiction, a history of trauma, or other psychiatric diagnoses. She’s gritty, brassy, and doesn’t hold back on telling you exactly what she thinks—and in the most simple and sometimes graphic terms.
“Normally what I consider to be my area of expertise is addiction in its multiple forms: Food, gambling, pot, porn, pills, sex…the whole gamut!”
Chauppette says addiction was on the rise among the general population as well as in people living with HIV (PLHIV), even before COVID-19. “In Los Angeles, methamphetamine remains the nightmare drug of choice for many of my HIV-positive patients. It is also the drug that has brought many of my patients to the world of HIV due to the hypersexuality and wild abandonment associated with the drug’s use.”
“I was talking with someone last night who had come home from not the bathhouse, because those are closed, but the underground bathhouse. And I said, where have you been, I’ve been looking for you for two days. ‘I was doing quaran-tina.’ Meaning, you know, party and play [PNP], but mostly with meth. Quaran-tina is just their wordplay with PNP plus the quarantine.”
Another form of addiction burdening our community is sex addiction, she says. “This is a more difficult form of addiction to treat as we possess the ‘drug’ 24/7—it is free, and often does not even require other human contacts. Your hand can be a form of addiction—meaning masturbation.”
Chauppette says that you can’t really work in addiction competently unless you understand other co-occurring disorders, “especially PTSD, bi-polarity, ADHD, some schizophrenia, and some personality disorders.”
“Historically, mental health folks like me don’t interact with the treating psychiatrist of the patient that we share, which is insane to me. So when my patients have their video Zoom conference call with their psychiatrist, I’m usually on that call. Because I’m going to be able to articulate what is really going on, easier and quicker, so that that ticking clock that we know has to be done in 20 minutes can actually be used with some efficacy. And most of my patients are happy to have me on the phone because they’re embarrassed about some of the stuff they did; you know, all the guilt and shame. I just cut to the chase, tell them what I’m going to say before I say it, so we have a prep call before I get on the phone with the doc and them. So they can trust me. I’ve got the facts, I’m not going to blindside them.”
She works closely with their HIV docs and is sometimes on those calls as well. “Usually, before COVID, I would meet them there and go in with them to see their HIV provider. Because a lot of them get in there and get anxious. They don’t want to disappoint the provider. They don’t want to say, ‘Look, I slipped again and had a PNP event, and I’m thinking maybe I should get checked for everything, STD-wise.’ Or, ‘My partner wants to go on PEP. He’s out in the waiting room; can you help him get on PEP today, because we hooked up last night?’
“So it’s a lot of what I call therapy-plus case management that I do. And I try to do integrated work…I think it’s unethical to work as a solo provider without talking to the major players who are also treating this patient. It’s more work, but I get better outcomes.
“My patients are burdened with significant addiction—multiple entities in an obsessive-compulsive way—and they also have concurrent psych [issues], or they’re chronic relapsers, and no one can figure it out. ‘What the hell, he seems to be trying, authentically, to stop using, or slow his roll, but he just can’t get it.’ We’ll then try to figure out what co-occurring psych is going on, because it’s almost always there…missed, over and over and over again. And then I determine whether or not I think at this level of severity of addiction whether or not they should go into an inpatient setting, to just put some geography between the body and the mind and the dealer and the hookups and the cell phone. Referrals come from different directions. Drug treatment programs out here will sometimes call me. They’ll hire me and say, ‘We’ve got a chronic relapse. We love this woman—or this guy, whoever it is—but we’ve done everything we know to do. Can you take a look at what we’re missing?’ And usually it’s major psych.
“I’ve seen thousands of patients with serious psych, usually multiple psych. ADHD, PTSD, bipolar disorder are the common three. And then of course HIV and hep C, which in my world is the least of the problems. Many of them got to the world of HIV behind undiagnosed and untreated psych. And when I say psych, I mean, addiction is a psychiatric disorder. Addiction can run solo by itself, but almost always there is an additional co-occurring psychiatric disorder, like the ones I’ve mentioned.”
It’s possible you can have all three, says Chauppette, but it’s treatable. “You just have to have a provider who gets you, gets your community. One of the blessings I have is that I’m part of the LGBTQ community, so I’m already in the door so to speak, and I know the culture. Even though I’m not male, I’ve seen so many gay male patients that I feel like I know it pretty well. So yes, it sounds overwhelming when you hear it, but a good provider can navigate it when he or she is really skilled and cross-trained, and willing to do the case management piece of talking to the doctors, the psychiatrists, the therapist if there is one, the case manager, and most importantly the HIV doc as well.”
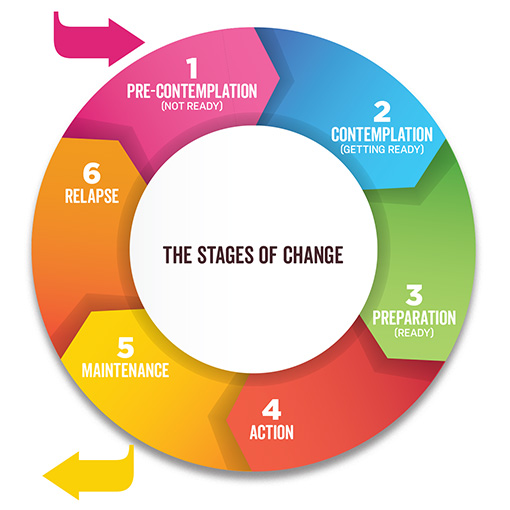
Chauppette employs the “stages of change” model when talking and working with patients, “to find out where they really are, as opposed to where I would like them to be.” According to Elizabeth Hartney, BSc, MSc, MD, PhD, the “stages of change” or “transtheoretical” model is a way of describing the process by which people overcome addiction, and “provides a useful way of understanding the process of change and gives a structure to how changes in addictive behaviors can be encouraged and managed.” There are variations on the model but it is essentially made up of four stages: Precontemplation, contemplation, preparation, and action. (Maintenance and relapse are also sometimes included as additional stages.)
Chauppette says she finds the evidence-based treatment that is appropriate for the level of change where her patients are at, and meets them there to develop a rapport and to try to minimize “wreckage accumulation,” while she tries helping them “move further down the chain of behavior change.”
“One of the mistakes we make as providers, I think, is that we overshoot readiness. Patient readiness is usually much less, no matter the problem—HIV, hep C, addiction, bipolar disorder. They’re usually not at the place yet where they are ready to see a psychiatrist, who of course is gay-friendly, HIV-knowledgeable, understands addiction—which we think is yes, yes, and yes, but is usually no, no, and no, that they have training in that area. So the stages of change model is kind of like a navigator for me…and I teach it to my patients. They like to use it. I’ll ask, what stage of change do you think you’re in for the nicotine dependence? And they’ll say, ‘Oh, I’m in pre-contemplation,’ which means don’t talk to me about it, I don’t want to hear about it, I’m gonna smoke on my deathbed. All the tools that I use, I try to teach them how they can use them…it gives them a roadmap, because they feel lost most of the time.
“If a patient is in the pre-contemplation or contemplation stage of change, one of the evidence-based treatments recommended is harm reduction. For example, a patient might not be ready or willing to use condoms even in a high-risk setting or discontinue drug or alcohol use, so we discuss PrEP and PEP as an urgent priority to keep the HIV-negative [person] just that—negative. Behavior change is a slow process that takes significant time, attention, and a lot of trial and error. I refer to my clients as patients as I want them to understand that we will both need to be patient in our work together. I am also a proponent of addiction medication. I have seen my patient’s chances of success increase significantly when we add to their recovery program MAT (medication-assisted therapy). Some examples are Suboxone, Vivitrol, and Campral. When a patient is in early recovery from addiction, and especially when it co-occurs with other major psychiatric disorders, the addition of MAT offers them a brain-based form of support.”
As a self-identified member of the LGBTQ community, Chauppette says that early in her career she felt a loyalty to her “brothers and sisters to help them in our fight to live dignified, authentic lives.” While completing her doctorate in Los Angeles, the HIV epidemic raged.
“I knew I always wanted to work with the diseases of our time—HIV, HCV, addiction. My brothers were dying horrible deaths, many alone, afraid, dealing with dying and death. For some, their own internalized homophobia was being fueled by ignorant and shame-based statements like ‘HIV is a message from God that your sexual orientation is the reason you have HIV and are suffering.’ ‘Leading a gay lifestyle is immoral.’ So, during my doctoral work I started treating HIV-positive heterosexual and gay/bisexual men, and trans women. For most, if not all my patients, even before their HIV-positive status, psychological suffering had been enormous and was now simply devastating.”
The LGBTQ community is exhausted but still fighting, says Chauppette. “Our heavily fought for gains are again in jeopardy. There is a push to move us back into the closet or require us to just settle for being ‘tolerated.’ We are not having it ever again, so we soldier on. We are indeed strong given the minority stressors we have and continue to face daily. Using addictive objects like drugs, food, pornography, chemsex, [and others] for attachment and coping is clearly dysfunctional and I hope as a community we can find other ways of coping that do not fulfill society’s expectations of us (i.e., to be self-destructive, hypersexual, irresponsible, etc.).”
For her trans patients, their journey is even more painful, she says. They are more heavily judged, and as they like to remind her, they reside in the “caboose of the LGBT train.”
“My transgender patients face sexual and physical violence, murder, verbal and non-verbal disrespect, housing and work discrimination, and mental and physical health ignorance and insensitivity. It is just awful.” She implores us to treat our transgender community members with kindness, support, guidance, and respect. “My transgender patients of color face even more challenges given their desire to live authentically atop the culture mandates from their ’hood.” She says she works closely with them to help them live authentically and dignified. “I help them see that the rudeness and lack of sensitivity from others should be addressed, but not in an aggressive manner. I teach them not to be ‘played’ and not to be messy even when the messenger is a mess. It is beneath them to become messy too. We practice ways to respond that permits them an option when they feel disrespected, and how to get their needs met without alienating others. As Michelle Obama says, ‘When they go low, we go high.’”
“There are many things we can do!” exclaims Chauppette when asked what we can do as a society to address mental health and addiction. “First, we must educate ourselves about mental illness and know that addiction is a mental illness. We need to understand that there is a genetic load [the presence of unfavorable genetic material in the genes of a population] for many mental illnesses and certainly for addiction. Addiction rarely occurs without the presence of other psychiatric illnesses. Understand…that addiction and other psychiatric disorders should not be shamed or judged. I tell my patients there is no shame in either, except knowing [that] you might or do have them and not get help. That choice may be based in shame and as a result you will stay sick and your life will not be yours. We need to stop using terms like addict, crazy, hype, and junkie so that people who need help cannot be turned away from seeking help. Seeking help is a sign of strength, not weakness. For those of us who are out about our addiction or mental health history, I commend you. Remember, people cannot shame us if we do not have shame ourselves. I would like to respectfully request that as members of the LGBTQ community we recognize that during our struggle we might have gone too far with PNP. Often it is a reaction to our own internalized homophobia, our rage as to why we are viewed as “less than,” and a derailment from our psychic pain. Leading authentic lives is the goal, but that should not include self-destruction.”
If you know someone who is struggling with addiction or mental health issues, there are lots of dos and don’ts, says Chauppette. “Do not be harsh with them. Talk to them from your heart and your head. Recognize that they are sick, not ‘bad.’ Recognize they are lost and that you must earn their respect by giving them respect, and not pushing them to do things that they are not ready to do.” She encourages her patients to Google search celebrities with addiction, bipolar disorder, or ADD/ADHD, to help them see that they are not alone, and that even very successful people can have these burdens.
“Teach them the drug or object of over-attachment is not the problem. Transference of addiction is the norm. That what they are attached to is fulfilling a need. I always teach patients that there is function in dysfunction! That means there are underlying psychological needs [being] addressed, albeit in a dysfunctional way, by using the form of addiction they are burdened with. Help them understand that they are not bad human beings but that the illnesses they are likely burdened with can make them engage in self-defeating behaviors.”
Chauppette says to let them know who can help them if and when they wish to take a time-out, or get a knowledgeable professional to help. “Do not have rescue fantasies or a need to be needed. If you like drama, you will likely be unable to help them. Be patient with strong boundaries. Speak truth and explore resistance. Do not enable. Do offer a more realistic option instead of abandoning them. For example, if someone you care for is in withdrawal, instead of giving them more alcohol or drugs or money for either, call paramedics instead. Do not be fearful of their anger. Remember, if you are healthy yourself you will not enable them.”
As for the pandemic, Chauppette says, “I’m not seeing much COVID in my HIV-positive patients. Most of them, their immune system is probably stronger than it’s ever been, because of the meds.
“Honestly, I don’t worry about HIV anymore, in terms of lethality. It’s the easiest to treat—to me addiction is the hardest to treat, and co-occurring mental illness is second in terms of difficulty to treat. HIV, you just need to swallow the pills, for the most part, right? Been there, done that; it’s old news to them. The only thing they complain about is, ‘It doesn’t give me anything, doc.’ I say no, it’s just keeping you alive. Hello? It’s keeping you alive, and do you want to stay alive?”