Held just before the start of the conference, the Pre-CROI Community Cure Workshop provides HIV cure research education and fosters dialogue between biomedical HIV cure researchers and community members, with the goal of promoting meaningful community involvement in HIV cure science.
During the workshop, an underlying theme emerged around the need for early community engagement while HIV cure-related research is still in the lab, the pre-clinical phases of the pipeline. Current engagement efforts must be demographically and geographically expanded, with a focus on key populations, and must be well funded and not approached as an afterthought. And incorporating social and behavioral research throughout the research enterprise as more clinical trials begin to investigate potentially curative therapies will be paramount for the field.
The 2023 Community HIV Cure Workshop was sponsored by Treatment Action Group (TAG), AIDS Treatments Activists Coalition (ATAC), AVAC, BEAT-HIV Community Advisory Board, CRISPR for Cure Collaboratory, DARE Community Advisory Board, Enterprise for Research and Advocacy to Stop and Eradicate HIV (ERASE-HIV), European AIDS Treatment Group (EATG), HOPE Collaboratory, I4C Collaboratory, National Minority AIDS Council (NMAC), PAVE Collaboratory, REACH Collaboratory, RID-HIV Collaboratory, and the University of Washington/Fred Hutch CFAR Cure Scientific Working Group.
Among the workshop highlights:
Morning Session
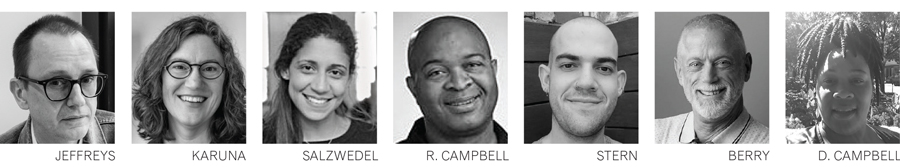
Treatment Action Group’s (TAG) Richard Jefferys and researcher, educator and activist Liz Barr provided an overview of the current landscape of HIV cure-related research. Since 2014, TAG has maintained a listing of HIV cure-related clinical trials and observational studies. As of February 2023, there have been 93 interventional trials (90 adult and 3 pediatric), and 38 observational studies (37 adult and 1 pediatric). Of those, 34 involved analytical treatment interruptions (ATIs). Most studies have been conducted in the Global North, and the majority (69%) obtained some community input. These statistics underscore the urgency of implementing HIV cure clinicals in resource-limited settings. Obtaining community input in research protocols will ensure that these protocols are community-friendly, as well as ethical and indicated for specific international populations. To date, over 14,000 people with HIV have participated in HIV cure-related studies, most of whom are men. For more information about demographics of participants in HIV cure-related clinical research, GO TO treatmentactiongroup.org/cure/resource-on-the-demographics-of-participation-in-hiv-cure-related-clinical-research/.
Shelly Karuna, Chief Medical Officer at Greenlight Biosciences, discussed ATI studies in Antibody-Mediated Prevention (AMP) trial participants. Two studies were described: HVTN 704/HPTN 085, occurring in the Americas and Europe in men who have sex with men (MSM) and transgender people, and HVTN 073/HPTN 081, occurring in sub-Saharan Africa in heterosexual women. All participants started ART early and received a combination of broadly neutralizing antibodies. The post-AMP ATI trial in Africa (HVTN 805/HPTN 093/ACTG 5393) began in early 2020 after extensive stakeholder engagement. The research team is following robust informed consent to facilitate decision-making. So far, of the 13 participants enrolled, one participant has maintained antiretroviral treatment (ART) suppression for over 18 months, and two additional participants have been off ART for 5–6 months. Dr. Karuna emphasized the possibility of conducting ATI trials safely in Africa. ATI trials require meaningful early stakeholder engagement and input to ensure that they remain community-friendly and ethical, no matter the specific context of any given country or group of potential participants.
Jessica Salzwedel (AVAC) moderated a panel discussion on community engagement for studies involving ATIs. Panelists included Michele Andrasik (HVTN), Gail Brocher (HVTN), Krista Dong (Ragon Institute), Udom Likhitwonnawut (independent consultant, Thailand), and Kenly Sikwese (AfroCAB). They discussed balancing participation while ensuring adequate safeguards, illustrating the need to maintain quality community engagement in HIV cure trials. They also questioned how in the era of Undetectable = Untransmittable (U = U), we discuss stopping antiretroviral therapy with potential participants. The panel emphasized the need to integrate socio-behavioral science studies that engage with HIV care providers and local ethics review committees, and acknowledged the role of partners, including referral for pre-exposure prophylaxis (PrEP) for partners without HIV. To design ethical studies, panelists stressed the need to engage communities early and often. We must understand participants’ needs and perspectives if we are to design human-centered clinical trials with analytical treatment interruptions.
Russell Campbell and Brian Minalga provided an overview of the Office of HIV/AIDS Network Coordination (HANC). Founded in 2004, HANC’s mission is to support the science and operations of the HIV/AIDS Clinical Trials Networks by increasing efficiency and resource sharing. HANC also coordinates critical activities across the networks and research and advocacy. HANC created a Representatives Studies Rubric (RSR) to guide and monitor enhanced representation in clinical research (e.g., age, drug use, ethnicity, gender, pregnancy, race, sex assigned at birth). A number of community resources are available through HANC, including guidance on how to review clinical trial protocols, a bill of rights and responsibilities for study participants, mentorship programs, and the Red Ribbon Registry. The HANC Webinar Library is at hanc.info/resources/webinars-and-presentations.html.
Afternoon Session
Jared Stern (Fred Hutchinson Cancer Center [Fred Hutch]) presented on the effects of long-term ART on the HIV reservoir (excerpts from the presentation appear in the March+April issue, “What makes HIV such a retro-virus?”). Dr. Stern described through an extended metaphor of a cookbook to help people understand the mechanisms of HIV persistence in people on suppressive ART, as well as ways ART changes the composition of the HIV reservoir over time. HIV establishes a chronic infection in T cells, (known as the reservoir), stressing that some viruses are more active than others. While on ART, active HIV-infected cells are cleared faster by the immune system than the inactive cells, resulting in the HIV reservoir becoming less active over time. Dr. Stern concluded that differences in the composition of the HIV reservoir may require tailoring different HIV cure interventions.
Jeff Berry (The Reunion Project) moderated a panel discussion on long-term survivors (LTS) and HIV cure research. Panelists included community members and researchers Bill Hall (Seattle), Pat Migliore (Seattle), Jared Stern (Fred Hutch) and Andrew Clark (ViiV Healthcare). The panel brought up the differences between LTS who were diagnosed with HIV at birth and people who are aging with HIV. Strategies to engage (LTS) in HIV cure research were explored. The role of medical mistrust in clinical research was acknowledged, together with the need to engage LTS communities in defining research questions. Ensuring a broad and diverse engagement of all LTS will enrich existing HIV cohorts.
Danielle Campbell (BEAT-HIV Collaboratory) noted that 51% of PLWH are women, presenting a community call to action to prioritize inclusion and enrollment of women in HIV cure research. She called for full support of women’s bodily autonomy and decision-making processes, considering women’s sexual and reproductive freedoms, providing no-cost contraception and ensuring representation and enrollment of women at all phases of research. Involving more women and communities from the Majority World (also known as the Global South) is called for, including socio-behavioral research to understand and address barriers to women’s enrollment, utilizing benchmarks for enrollment, engaging community-based organizations to assist with accrual and retention and performing sex-based analyses. For more details about the call to action, GO TO bit.ly/call-to-action-women-in-HIV-cure-research.
The pre-CROI Community HIV Cure Research Workshop made clear that all these years into the AIDS pandemic, real diversity in HIV clinical research is desperately needed, with social justice for all people who are disparately affected by HIV. Further community input is needed to ensure that clinical trials remain ethical, centering around the priorities of people living with HIV, and that socio-behavioral studies are embedded with biomedical interventions. Without these elements, clinical trials, already struggling to accrue and retain participants, will result in insufficient data that represent all people affected by HIV.
For more information about the 2023 Pre-CROI Community Cure Workshop, including recordings and slides from each presentation, go to Treatment Action Group—2023 Pre-CROI Community HIV Cure Research Workshop: treatmentactiongroup.org/webinar/2023-pre-croi-community-hiv-cure-research-workshop.
About the writers
Karine Dubé is an associate professor at the University of California San Diego School of Medicine and Global Public Health. She is a socio-behavioral scientist focused on integrating a patient/participant perspective into HIV cure-related research in the United States and South Africa, and is a member of the Delaney AIDS Research Enterprise (DARE) Community Advisory Board (CAB). She also leads the BEAT-HIV Social Sciences Initiative and is a member of the Global Gene Therapy Initiative (GGTI).
Lynda Dee co-founded AIDS Action Baltimore in 1987. She has worked with academia, industry and government to expedite drug development and provide access to HIV medications. Dee has served on many advisory boards, including various FDA approval panels, NIH Advisory Boards and industry CABs, and is a founding member of the AIDS Treatment Activists Coalition. She has also worked in the HIV cure research arena as co-chair of the Martin Delaney Collaboratory (MDC) CARE CAB, co-chair of the amfAR Cure Institute CAB, and is now the DARE MDC Community Engagement Coordinator.
Jeff Berry is executive director and co-founder of The Reunion Project, the national alliance of HIV long-term survivors, and serves as National Steering Committee Chair. Berry most recently served as chief editorial officer of TPAN and editor-in-chief of Positively Aware, serving as editor from 2005–2022. He is the inaugural chair of the CRISPR for Cure CAB of the Martin Delaney Cure Collaboratories, and a member of the Illinois Commission on LGBTQ Aging, the Community Collaboration Board (CCB) of the Third Coast Center for AIDS Research (CFAR), the Fair Pricing Coalition (FPC), and the AIDS Treatment Activists Coalition (ATAC).
Michael Louella is proud to serve as a co-chair for the DARE Community Advisory Board. He has worked in HIV treatment research for 23 years, engaging communities affected by HIV in Seattle and across the U.S. in clinical trials towards the treatment and potential elimination of HIV from the body. He joined the defeatHIV Martin Delaney Collaboratory as its Community Engagement Project Manager in 2013, focusing his efforts around cell and gene therapies for HIV cure. He serves on the steering committee for The Reunion Project, working to develop more events for HIV long-term survivors. Recently he joined the Global Gene Therapy Initiative, an alliance of key stakeholders including clinicians, scientists, engineers, advocates and community members brought together to enable access and implementation of gene therapies as curative medicines for presently incurable diseases in Majority World countries.