The sudden emergence of the mpox virus (previously known as “monkeypox”) has been explicitly felt by queer and HIV communities. Stigma, misinformation and fear are reminiscent of the U.S. HIV/AIDS epidemic, and the even more recent COVID-19 pandemic. People living with HIV are especially vulnerable to both the emotional anxieties and to acquiring the disease itself. As a Black queer person (and therapeutic provider), my peers, colleagues, clients and I have had many conversations about the mpox outbreak, its effects on our social and sexual health, and where and how to seek health care. I noticed early in this outbreak that fear and anxiety were especially palpable among queer people and people living with HIV.
Black and Brown queer people especially feel vulnerable in times of disease outbreaks as we have seen priority access to preventative and treatment interventions offered to White queer people over our communities. Several of my clients and team members feared they would be exposed to MPX before their social and intimate partner circles were offered access to vaccines. And recently we’ve begun to see data published by big cities like New York, Atlanta and Washington, D.C. demonstrating that Black and Brown gay, bisexual and other men who have sex with men are disproportionately being diagnosed with mpox, while a majority of vaccinations have gone to White gay and bisexual men, even as Black and Brown men reported actively trying to get a vaccine appointment.
A lot of my work recently has been teaching patients, community member, and friends how to maintain their emotional health and well-being while also working harder than most to seek equitable access to preventative health care and treatment intervention for mpox. I am writing this piece in hopes that it will continue our communities’ hard work to secure our emotional and physical health, and to offer some ways we can each hold that onus.
Reality test: Do I have real reason for concern?
Self-reflection is powerful, and a good place to start in managing fear and anxiety. Ask yourself the following:
“Are my worries rational?”
“Is this a projected or actual danger?”
“Am I able to keep myself safe?”
“What tools do I need to keep myself safe and free of worry?”
This is called reality testing. Reality testing is an objective assessment of an emotion or thought against real life. Is this thought based on reality? We have very creative minds that are capable of coming up with all types of scenarios. Understanding what is real, as in what is happening to you in the present, versus what could happen, is a thought process most likely to keep you from creating unnecessary worry or anxiety for yourself.
So if you are concerned, even deeply fearful of contracting mpox, one thing to do is to breathe and ask yourself, why am I afraid? Have I actually done anything to be potentially exposed to mpox?
Seek out reliable sources of information to assess your real risk.
Another way to combat fear and anxiety is to seek out reliable information and to be proactive about your health. This can help create a sense of safety and empowerment. Fear and anxiety are greatly reduced when we as people feel safe. Reading some of the risk assessments from trusted sources such as the Centers for Disease Control and Prevention (CDC) or your local health department is a good way to assess whether your anxiety is well-founded, or whether you may be triggered by the last few years of the COVID pandemic, or by living with HIV in a world that regularly stigmatizes us, or blames people living with HIV, people of color, immigrants or poor people for infectious disease outbreaks.
Get vaccinated against mpox if you are able.
For some people, that can mean seeking out getting vaccinated against mpox as a way to decrease anxiety around disease acquisition. I received the first dose of the MPX vaccine in July 2022 through Fulton County Board of Health in Georgia, where I live. Access to MPX vaccines was very limited in the first few months of the outbreak in the U.S., with the bulk of available vaccines being concentrated in urban areas or more vulnerable populations, including people living with HIV. In my own experience, I was unsuccessful getting a vaccine appointment for the first month I attempted to secure one. Open appointment links were full in a matter of minutes, representing hundreds of vaccine slots.
Part of health care is not just getting shots or pills, but also getting accurate health information from providers, so feel empowered to ask any and all questions, and to take your time until you feel comfortable.
Raise any questions or concerns you have with a medical provider.
Upon receiving my mpox vaccine dose I met with a provider who answered all my questions about the vaccine before I received my dose. I highly encourage readers, especially anyone anxious about vaccines or needles, to prepare for your appointment by writing down your questions and bringing them with you to your appointment. Part of health care is not just getting shots or pills, but also getting accurate health information from providers, so feel empowered to ask any and all questions, and to take your time until you feel comfortable.
During my vaccination appointment, my vaccine provider, an infectious disease physician, answered my questions. She told me the mpox vaccine is a series of two shots separated by 28 days, with full protection at two weeks after the second dose. It is uncertain if there is partial protection after one dose. The vaccine is either administered through a small needle into the fleshy or fatty part (tissue) of the back of your arm, or just underneath the skin. I was told I would feel a slight prick followed by some soreness. The soreness or itchiness could last a few weeks. Mine lasted three weeks and appeared as a hard, warm, red bump at the injection site. The bump was expected and is not the result of an allergic reaction. Some people feel tiredness or fatigue shortly after receiving the dose, explained my provider. I did not, however. Having this information, knowing what to expect, was incredibly helpful, as I have been known to become anxious when faced with health concerns. You won’t lead yourself down a rabbit hole of what ifs if you know what to expect.
During my appointment, I learned mpox originated in Africa, and historically had been contained to that continent. There have been some intermittent outbreaks here in the U.S., with the last outbreak associated with the importation of animals from Africa. The current outbreak is of a different strain from the original strain in Africa and is thought to be transmitted through skin-to-skin contact. You can visit the CDC’s website if you want to track the number of cases, learn more about the history, symptoms, and spread of disease, or how to lower your risk during sex, at cdc.gov/poxvirus/monkeypox.
This resource was shared with me by my provider during my vaccine visit. She went on to explain that mpox is not spread so much by the exchange of bodily fluids, but more by bodily contact (touching, rubbing, kissing) as well as by surface contact, for example, the sharing of bed sheets, towels, and equipment that has been exposed. Hot water is enough to kill the virus, so no need to trash your belongings if you have been exposed to mpox; just wash them well in very hot water. Again, information and care instructions are helpful in reducing fear and anxiety surrounding mpox. This information may also help you build confidence in your ability to keep yourself safe.
In review
So, let’s briefly recap. To manage fear and anxiety, especially around health concerns, first self-reflect and reality test. Seek out accurate information and guidance. Love on yourself by being confident in your abilities to manage negative or panic-based thoughts and pause emotion to make sound decisions. Invest in being proactive with preventative care like vaccination and treatment. You are your best coach, friend, advocate, and leader. Having information, an ability to use that information prior to making decisions, an understanding of your emotions and thoughts, and skills in managing them, will keep you safe, well, and healthy.
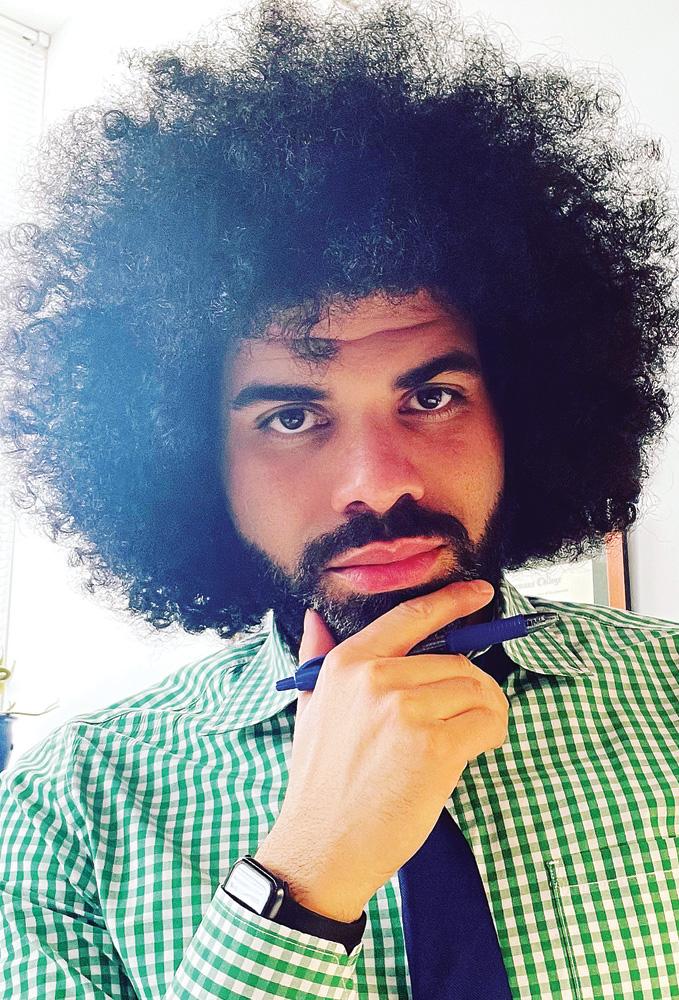
Dr. Nathaniel Currie, DSW, MSW, LCSW, is a clinical social worker and educator with more than 14 years of social work experience in mental health and HIV. He is an associate professor of social work and social justice at the Whitney M. Young, Jr. School of Social Work at Clark Atlanta University. He is an active social science researcher, keynote speaker and yoga instructor. He and his terrier, Jackson, and French bulldog, Sebastian, split their time between Los Angeles and Atlanta. Follow him on Twitter: @AskDoctorNate.


