A clinician talks about linkage and retention in care
Here in New York, only 66% of those living with HIV are linked to care and 57% are retained in care, according to the 2013 New York State HIV Care Continuum (or Treatment Cascade). The cascade also shows that only about half of people living with HIV in New York achieve viral loads less than 200.
We are all aware of the benefits of being on ART (antiretroviral therapy), and that persistent viremia (having detectable viral loads) can cause ongoing inflammation leading to negative consequences such as cardiovascular disease, yet many patients are not engaged in care and their virus controlled on medications.
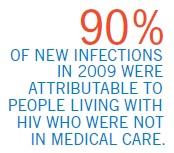
Furthermore, not being on treatment and achieving undetectable viral load also increases the risk of transmitting HIV. In 2015, the CDC published a study estimating the number of HIV infections from people at each level of the Care Continuum in the U.S. According to the study, more than 90% of new infections in 2009 were attributable to people living with HIV who were not in medical care.
That means 9 out of 10 new infections could’ve been prevented by getting people tested and diagnosed early, linking and retaining them in care, and helping them achieve virologic suppression through ART.
So why are people lost to care? A number of individuals are never connected to care in the first place after an initial HIV diagnosis. Regular testing and early diagnosis are great, but it isn’t very useful if nothing is done about it afterwards.
Some people who use home HIV testing kits may be reluctant to seek medical care after diagnosis due to stigma or fear. Others who test positive don’t seek care because they feel healthy and don’t want to get on meds, even though the current recommendation is to treat everyone regardless of CD4 count, the earlier the better.
The view from one Center
Here at Gay Men’s Health Crisis (GMHC) where I practice, when an individual is diagnosed with HIV at our testing center, he/she is physically walked over by a staff member to a clinic to be connected immediately to care.
Once linked to care and put on ART, a number of individuals are not retained and engaged in care. According to studies, some demographic and clinical factors associated with missing clinic appointments include race (African American), younger age, low income, less education, lack of insurance, injection drug use, psychiatric issues, detectable viral loads, high CD4 counts, and CD4 counts less than 200 (AIDS diagnosis).
Sometimes when people don’t feel sick they don’t seek regular medical attention. But on the other hand, those that feel too sick may not have the energy to attend a medical appointment.
Patients have also identified social and cultural factors which cause them to miss appointments, including lack of child care, conflicting work schedule or social appointments, lack of transportation, family illness, stigma, fear, and cultural beliefs. Then there are those that simply forget. Some of my patients miss appointments because they live too far away from the clinic, yet others choose to travel long distances to see specific providers. Other common reasons that I see in my patients include being too sick, lack of transportation (or not enough money for public transit), forgetfulness, hindrance by bad weather, and simply because they didn’t want to see the provider. I had a patient who disappeared for months, whom I later found out was incarcerated. This individual subsequently came back to see me after release.
Improving retention
What can we do to improve retention? First, we have to truly understand the reasons why someone would miss appointments or is lost to care, especially the socio-cultural factors, and come up with individualized solutions. There have been different interventions used to help improve retention, such as appointment reminders, HIV education, social work and case management, verifying and updating the patient’s contact information at each visit, and providing services for mental health, nutrition, housing, and substance abuse treatment. A multipronged approach seems to be the most effective, addressing different aspects of a person’s daily life.
Here at GMHC, clients have access to a variety of supportive service programs such as care coordination, mental health support, food and nutrition, case management, advocacy, employment and legal services, and complementary wellness services such as massage and acupuncture.
Keeping those living with HIV in ongoing care can be a difficult process, but it should be a priority. Sometimes it is as easy as providing a subway pass to help patients keep their appointment. But oftentimes it really does take a village working together to keep someone engaged. Successful retention will result in improved HIV-related clinical outcomes, reduce the risk of treatment failure, and improve the relationship between patients and providers.
Christopher M. Nguyen, PharmD, AAHIVP is an HIV and hepatitis C specialty pharmacist for Walgreens/Duane Reade in New York City and currently provides care at Gay Men’s Health Crisis. He works directly with clients on HIV-related issues such as adherence and medication management, and provides consults for local practitioners on drug interactions, dosing adjustments, and HIV and HCV regimen selection in co-infected patients. Dr. Nguyen served as the pharmacist for this year’s Positively Aware Annual HIV Drug Guide (March+April).


