Looking After Your Heart
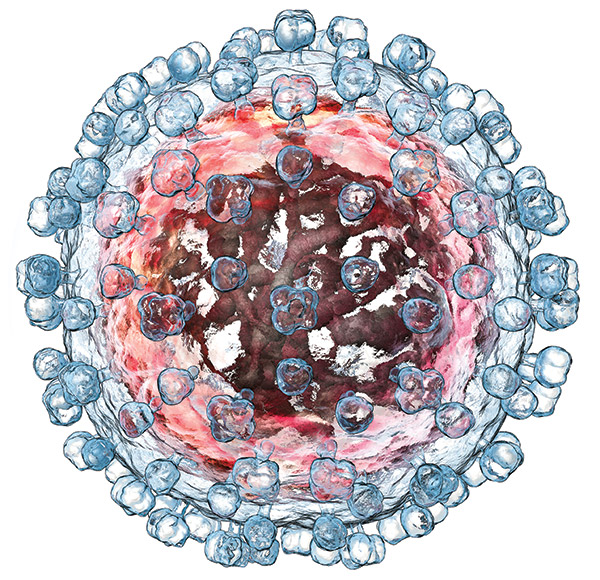
Your heart and your circulation become some of the biggest areas of maintenance—and potential problems—as you get older. Abnormal lipid levels—cholesterol and triglycerides—raise the risk of heart attacks and other cardiovascular problems. People living with HIV are more likely to have abnormal lipid levels off HIV treatment due to the virus. Even on treatment, a high proportion of people living with HIV (PLWH) have low levels of “good” cholesterol, raising the risk of heart disease.1
Maintaining healthy cholesterol levels—keeping total cholesterol below 200 mg/dl and the ratio of total cholesterol to HDL cholesterol below 5 to 1—reduces your risk of heart disease. If lifestyle and diet changes aren’t getting your numbers into the right range, it’s time to talk with your doctor about how your HIV meds might affect your lipid levels. Protease inhibitors may increase your lipid levels, whereas integrase inhibitors and newer NNRTIs such as rilpivirine or doravirine have less effect on lipids.
Your physician should calculate your 10-year risk of a heart attack or other cardiovascular problem, using your weight, age, blood pressure, and cholesterol scores. If you’re at high risk, your physician will prescribe a statin medication and set a goal for cholesterol reduction.
HIV also raises the risk of heart disease, especially in women and younger people. Some experts have suggested that the additional impact of HIV on the risk of heart disease means that everyone living with HIV should take a statin. The jury is still out on whether this is a good idea, and a big trial is running to answer the question. (See “Should you be taking a statin if you’re living with HIV?”)

HIV raises the risk of heart disease, especially in women and younger people.
Raised lipid levels are often accompanied by other problems—such as increased glucose, high blood pressure, excess fat round the waist, and a fatty liver—that also raise the risk of heart disease. This cluster of problems, described as metabolic syndrome, requires careful monitoring and intervention before it leads to type 2 diabetes, heart disease, stroke, or serious liver damage.
Metformin is usually the first option to manage glucose levels. Other drugs to manage glucose are less well studied in people with HIV, and may have problematic drug-drug interactions with some anti-HIV drugs.2 Whereas boosted protease inhibitors may increase levels of many drugs used to manage glucose, non-nukes such as efavirenz may reduce levels.
Smoking is still a major culprit in heart disease for PLWH, just as for the rest of the population. Kery Althoff of Johns Hopkins University, Baltimore, looked at the medical history of nearly 30,000 people in HIV care in North America. She found that people who smoked were 80% more likely to have a heart attack than those who had never smoked. If everyone stopped smoking, around 40% of all heart attacks in PLWH would be avoided, she estimates.
Althoff also found high blood pressure and being overweight were major risk factors for heart attacks. All these factors were much more important than having a low CD4 count, a detectable viral load, or hepatitis C.3
Maintaining a healthy weight can become more difficult as you age, especially if you have a disability. Having a higher body mass index (a BMI above 30) increases your risk of heart disease.4 In the general population, people who are overweight are more likely to develop heart disease, develop it earlier, and spend more of their life with heart disease. It is unclear if the same holds true for PLWH, but weight gain after starting HIV treatment is associated with an increased risk of developing abnormal glucose levels, including type 2 diabetes (a major risk factor for heart disease).5
As you get older, your doctor should regularly ask about your ability to carry out the normal activities of daily life and take note of changes in your weight.
Your body begins to show its age
Signs of physical wear and tear are an inevitable part of aging, but for some PLWH, aging is accompanied by premature frailty and loss of muscle mass, along with other conditions.
Frailty manifests as weight loss, slowed walking speed, reduced strength, tiredness, and a lowered level of physical activity—a noticeable escalation of “not being able to do as much as I used to.” A Dutch study found that PLWH were more likely to be frail than their HIV-negative counterparts at any age, and that the condition was more common in people who had ever had an unusually low body weight. The study investigators concluded that “frailty may be a long-term consequence of having experienced advanced HIV disease.”6
Greater frailty places you at risk of falls. Injury in a fall can interfere with your ability to shop, cook, and carry out all the other tasks of daily life. It may affect your ability to work, isolate you from friends and neighbors, and lead to greater frailty in the future. Fractures are a common consequence of a fall in older people; in the worst cases, a broken hip can lead to hospitalization.
As you get older, your doctor should regularly ask about your ability to carry out the normal activities of daily life and take note of changes in your weight. Moderate exercise may improve your resilience if you are frail, but we know little about how much exercise is needed to improve quality of life or prevent greater frailty in older PLWH.7
If you are showing signs of frailty, your health care provider should take time to explore how exercise, diet, and other lifestyle changes could help you, and investigate whether you are taking any medications that might be contributing to your problems. Frail people tend to be taking more medications than others because of multiple health conditions, but we know very little about the effects of polypharmacy and drug-drug interactions on frailty in PLWH.8
These old bones
Frailty is closely linked to, but not the same as, bone loss. Thinning of the bones—osteopenia—can occur despite healthy muscle mass in middle-aged people and in people with an average body weight. In PLWH, a combination of long-term untreated HIV disease, alcohol, smoking, low vitamin D levels, and antiretroviral therapy can lead to a loss of bone mineral density, or bone thinning. After starting HIV treatment, PLWH tend to experience a pronounced drop in bone mineral density of around 2–6% in the first two years. More serious bone loss—osteoporosis—tends to affect women after menopause and older men.
There are lots of things you can do to strengthen your bones and ward off bone thinning. Make sure to eat foods rich in calcium, which makes new bone. Dairy, tofu, spinach, and broccoli are rich in calcium. A supplement may help you get the 1,300 mg a day recommended for women over 50 and men over 70. Men aged 50 to 70 with a risk of fractures should aim to get at least 1,000 mg a day. A supplement that contains a small amount of vitamin D may be helpful if you aren’t getting a daily dose of sunshine or if you aren’t eating dairy, eggs, fish, or liver.
Weight-bearing and resistance exercise, quitting smoking and drinking, and drinking less alcohol all help maintain bone mass. Guidelines say that your bone mineral density should be measured using a DEXA scan if you are a postmenopausal woman, a man over age 50, or if you may be at high risk for fractures based on your age, gender, weight, or smoking and alcohol history. Three months of glucocorticoid treatment would also indicate the need for screening.9
Treatment with tenofovir has been shown to result in greater bone loss than other drugs. A newer formulation of tenofovir, TAF, has been touted as kinder to the bones, but when researchers looked at whether people taking TAF had fewer fractures than people taking the older version of tenofovir (TDF), the evidence from clinical trials suggests that TAF only provides an advantage if it is being used with the boosters ritonavir or cobicistat.10 What’s more, when French researchers looked at everyone receiving HIV treatment in France between 2000 and 2010, they were unable to show that any HIV drug—including the older form of tenofovir—resulted in a higher risk of a fracture.11
Nevertheless, many physicians will advise switching away from TDF if you have a high risk of fractures.

Spinach, as well as tofu, broccoli, and dairy foods are rich in calcium.
Numerous medications have been approved for the treatment of bone loss in post-menopausal women and older men, but the only ones tested in PLWH are calcium and vitamin D, alendronate, and zoledronic acid. A trial of alendronate added to calcium and vitamin D showed that adding alendronate (Fosamax) improved bone mineral density but did not result in fewer fractures than calcium and vitamin D supplementation.12 A recent study either switched people away from tenofovir (TDF) or gave participants zoledronic acid (Reclast) while they took tenofovir. Zoledronic acid infusions resulted in substantial improvement in bone mineral density over two years, but the study found no difference in fractures.13
Guidelines recommend that PLWH with low bone mineral density or a risk of fractures should get alendronate (70 mg once a week) and receive monitoring for vitamin D levels.14
High blood pressure and being overweight are major risk factors for heart attacks. All these factors were much more important than having a low CD4 count a detectable viral load, or hepatitis C.
Neuropathy
Peripheral neuropathy (nerve damage in the feet, legs, and hands) may be caused by untreated HIV or past treatment with one of the old NRTIs—stavudine (d4T), didanosine (ddI), or zalcitabine (ddC). Peripheral neuropathy may also be caused by type 2 diabetes or by alcohol abuse. No treatment has been shown to repair nerve damage, so pain relief is essential, starting with over-the-counter painkillers and escalating to prescription painkillers according to the severity of pain. A skin patch called Qutenza, which contains capsaicin, the chemical that makes chili peppers hot, has been shown to provide moderate pain relief. Anticonvulsants or tricyclic antidepressants may also provide some pain relief.
Breathing difficulties
Chronic obstructive pulmonary disease (COPD) and emphysema are common problems for older PLWH. Both conditions lead to breathing difficulties and a loss of mobility, and COPD can become a progressive condition. Although smoking worsens both conditions, there’s some evidence that long-term HIV infection also increases the risk of breathing problems, emphysema, and COPD16, 17, 18, and these problems can begin to appear at a younger age in PLWH.19
Stopping smoking is the single most important thing you can do to avoid the development of COPD or prevent it from getting worse. Ask your health care provider what support is available to help you quit if they haven’t already suggested it.
Treatment of COPD is just the same for PLWH as for anyone else, with a word of warning: levels of fluticasone, an inhaled corticosteroid used in the treatment of severe cases of airway obstruction, can be raised by boosted protease inhibitors. Be sure that your primary care or emergency room physician checks for drug-drug interactions with HIV meds before giving you a systemic corticosteroid or theophylline to help your breathing.
Arthritis
Osteoarthritis (degenerative joint disease) is common in older adults. HIV does not increase the risk of osteoarthritis, but can cause some other forms of arthritis that lead to pain and swelling in the joints. These HIV-associated flare-ups of arthritis in the joints are usually temporary and can be treated with NSAIDS (aspirin, Advil, and others) or steroids. Some other forms of arthritis, such as psoriatic arthritis or rheumatoid arthritis, may require management by a rheumatologist.20
Fatigue, insomnia, and sleep apnea
Chronic tiredness in PLWH has many causes, including disturbed sleep, stress, depression, anemia, untreated hepatitis C or chronic liver disease, testosterone deficiency, or hypothyroidism. Sleep disturbance—either difficulty falling asleep or poor-quality sleep—is less likely to occur as a side effect of newer HIV drugs such as integrase inhibitors, but if you are experiencing problems, talk to your physician.
One problem that becomes more common in older people is obstructive sleep apnea. This is a condition in which the muscles of the throat relax during sleep, leading to temporary blockage of the airways. The blockage may last for only a few seconds, but it may occur frequently during sleep, leading to poor-quality sleep and daytime fatigue. The condition is more common in men, in older people, and in those who are overweight. Smoking and excessive alcohol consumption make the condition more likely too.

Regular dental exams are also important for spotting potential cancers in the mouth and upper throat.
Dentistry
Teeth are often neglected when thinking about aging and HIV, but one problem common to everyone as they age is declining dental health. These problems can be complicated in PLWH by a lack of HIV-friendly dental care within easy reach. A recent study in Texas showed that the need for dental care was especially acute among PLWH who had fallen out of care; more than half had an unmet need for dental treatment when they later turned up as in-patients at a Houston public hospital.15
Regular dental exams are also important for spotting potential cancers in the mouth and upper throat. The high prevalence of smoking and alcohol consumption among PLWH, together with human papillomavirus strains that cause some oral cancers, means that they are at higher risk of oral and pharyngeal cancers.
Careful management of blood pressure, lipids, kidney function, diabetes, and cardiovascular problems can play a part in preventing cognitive decline, along with cutting down on alcohol.
Neurocognitive impairment and dementia
Changes in concentration, memory, decision making, and attention span are a common feature of aging. Neurocognitive impairment—deficits in memory and thinking compared to others of a similar age and background—can range from mild to severe (dementia) and has many potential causes.
PLWH are not at higher risk of major cognitive impairment resulting from HIV. Other risk factors, such as severe kidney disease, obesity, long-term excessive alcohol consumption, depression, high blood pressure, cardiovascular disease, and type 2 diabetes, are likely more important.21 Having numerous health problems alongside HIV appears to raise the risk of cognitive impairment.22 Although some studies show subtle deficits in PLWH when compared to others of the same age, there is little evidence that cognitive impairment gets worse.23 The long-term implications of differences between PLWH and others are unclear.
Careful management of blood pressure, lipids, kidney function, diabetes, and cardiovascular problems can play a part in preventing cognitive decline, along with cutting down on alcohol. If HIV seems to be playing any part in cognitive decline, your doctor may suggest changing your HIV drugs to ensure that you are taking a combination that fully suppresses HIV in the brain and central nervous system. Abacavir, emtricitabine, raltegravir, and boosted darunavir penetrate the brain better than other HIV drugs.
Hepatitis C Virus (HCV): Co-infection with hepatitis C also puts PLWH at higher risk for chronic kidney disease.
Kidney disease
Our kidneys work less well as we age, but people with diabetes or high blood pressure are especially prone to loss of kidney function and kidney damage. HIV may also play a role, especially among African Americans, and so may some anti-HIV drugs. Co-infection with hepatitis C also puts PLWH at higher risk for chronic kidney disease.
Kidney damage caused by HIV can be limited by starting HIV treatment as soon as possible after diagnosis. For people who have suffered some kidney damage due to HIV, ACE inhibitors or angiotensin receptor blockers used for treating high blood pressure may be prescribed alongside HIV treatment.
Your physician should monitor your kidney function regularly, along with your blood sugar and blood pressure, and prescribe medication to manage your blood pressure, cholesterol, and blood sugar where needed.
If your kidney function is declining, some anti-HIV drugs should be avoided, especially if you are over 60 and have other conditions that increase the risk of kidney damage. Tenofovir (TDF), atazanavir (Reyataz), and lopinavir/ritonavir (Kaletra) should be avoided. The new formulation of tenofovir (TAF) is less likely to affect kidney function.24
Kidney damage caused by HIV can be limited by starting HIV treatment as soon as possible after diagnosis.
Liver disease
The main cause of liver disease in PLWH is co-infection with hepatitis B or C. Direct-acting antiviral treatment for hepatitis C (HCV) is recommended for all PLWH, regardless of liver disease stage, but HCV treatment is costly and access to treatment depends on health insurance. You can get more information on how to access HCV treatment from HELP-4-HEP, 877-435-7443.
Organ failure—the new transplant potential
When organs are failing, the transplant list is not an easy place to be. Recently however, new hope for people with end-stage organ disease emerged with the news that several research groups in the United States had carried out successful transplants of organs donated by PLWH to others with HIV who needed them. The HIV Organ Policy Equity Act of 2013 permits PLWH to donate kidneys or livers as part of a research study. The National Institutes of Health is running a large trial of kidney transplantation for PLWH, half receiving kidneys from donors with HIV. Heart transplants have also been carried out.
Many of the health problems that face older PLWH are the same as those faced by everyone else but may need HIV specialist input to get the most appropriate care.
Conclusion
Many of the health problems that face older PLWH are the same as those faced by everyone else but may need HIV specialist input to get the most appropriate care. See page 15 for more information on care providers.
If there’s one action point to take away from this article, it’s quit smoking if you can, and get help to quit. Smoking exacerbates many of the problems faced by aging PLWH. Heart disease, high blood pressure, breathing problems and chronic lung disease, gum disease, bone thinning and fractures, reduced kidney function, and cognitive decline are all more common in smokers and likely to be more severe. Medication to help you quit is available and greatly improves your chances of quitting. The National Cancer Institute provides an online tool to help you develop your plan to quit—view it at smokefree.gov/build-your-quit-plan.

Keith Alcorn
Keith Alcorn is former editor of aidsmap.com. Based in London, Keith writes about HIV, TB, and viral hepatitis. His cat Binks pays close attention.