The liver is the body’s largest internal organ, and is responsible for over 500 vital functions. It’s a remarkable organ that even has the ability to re-grow itself. The easiest way to think about the liver is as your body’s filtering system and warehouse. The liver filters everything we eat, drink, breathe, or absorb through our skin. It also stores nutrients like vitamins, minerals, and iron.
Other functions of the liver include:
• Clears out alcohol and drugs (both legal and illicit)
• Makes bile and helps digest food
• Manages fats and cholesterol
• Manages sugars
• Makes platelets that help blood to clot
A healthy liver is essential for a healthy life. Getting cured of hepatitis C (HCV) will stop the damage done to the liver, and may even lead to a reversal back to a healthy one, including minimizing the risk of liver cancer. Beyond cure, there are many things you can do to help your liver stay healthy.
Fibrosis and cirrhosis
Over time, HCV can cause damage to the liver, leading to fibrosis and cirrhosis. For people living with HCV alone, the scarring process is relatively slow: Without treatment, it takes an average of 20–30 years for fibrosis to develop into cirrhosis. HIV/HCV co-infection can speed up liver damage dramatically.
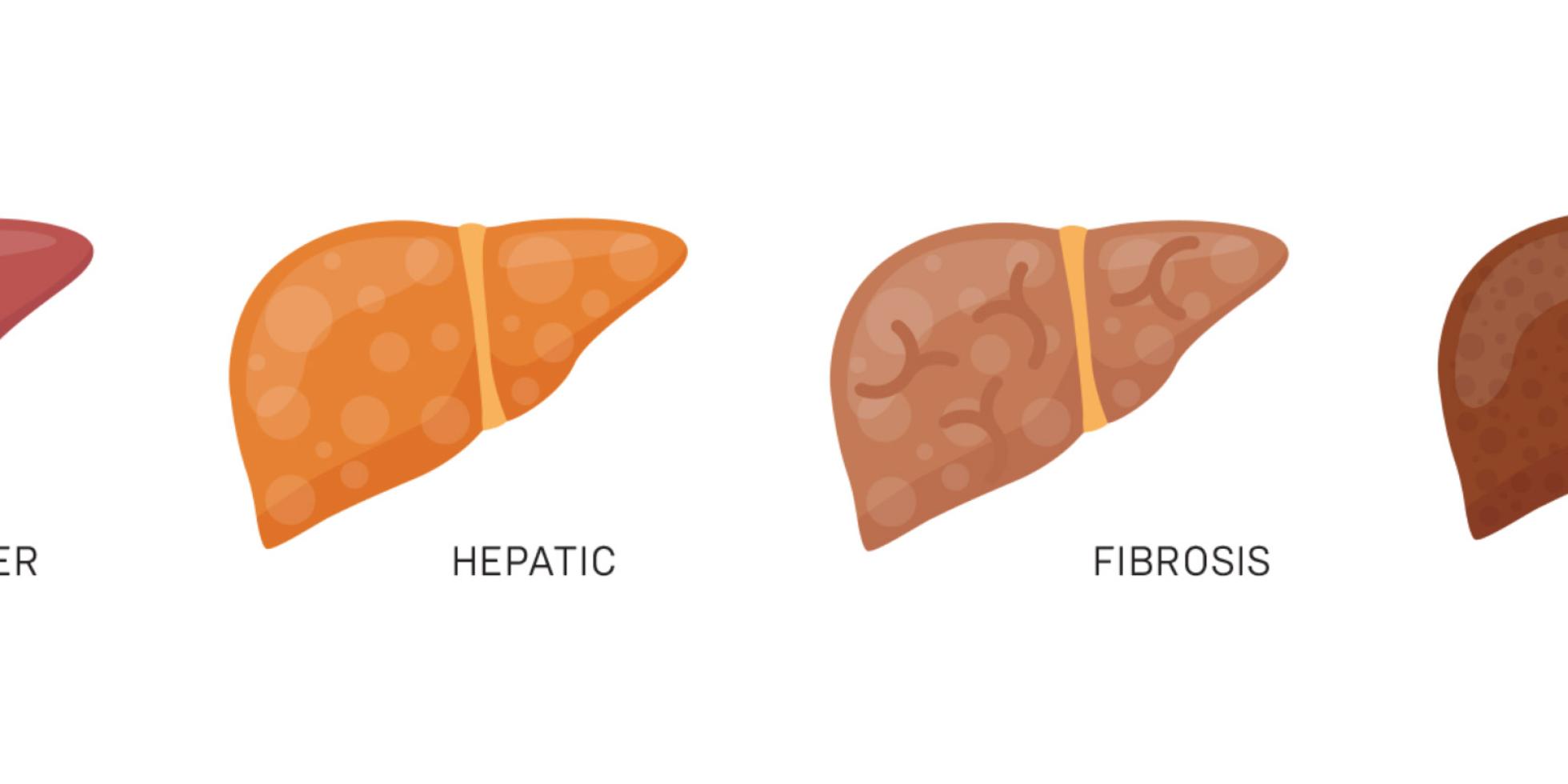
Fibrosis
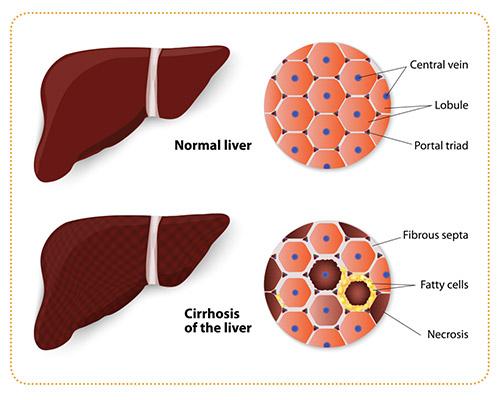
Chronic inflammation of the liver leads to the production of substances (collagen and other proteins) that can damage the liver’s cells. Over time, this damage can lead to scarring. Fibrosis refers to the development of scar tissue in the liver. In the early stages of fibrosis, the liver is able to perform its functions with relative ease. Over time, the fibrosis grows and the scar tissue spreads, stressing the liver and its ability to do its job. As the fibrosis and scar tissue expand, it can eventually lead to cirrhosis. The speed with which fibrosis develops is different from person to person, with several other factors that can speed it up.
Factors that influence the rate of fibrosis progression:
• Alcohol consumption
• Age at time of infection
• Co-infection with hepatitis B
• Co-infection with HIV
• Presence of other comorbid diseases (such as diabetes)
There are different ways your medical provider can measure fibrosis and cirrhosis, ranging from a liver biopsy (not done as frequently as in the past, but still the gold standard of measurement) to blood tests. Increasingly, there is a non-invasive (that is, no blood needed) means of measuring liver scarring called “transient elastography” (aka FibroScan), which is painless, fast and easy. While each of these tests are different, they all report their results in a similar way (see chart below):
Fibrosis scoring system
| SCORE | AMOUNT OF FIBROSIS |
| F0 - F1 | No to minimal fibrosis |
| F2 | Significant fibrosis |
| F3 | Severe fibrosis |
| F4 | Cirrhosis |
Cirrhosis
As the fibrosis progresses and the scarring covers more and more of the liver, it literally changes shape. This is called cirrhosis. Early cirrhosis, called compensated cirrhosis, can also be asymptomatic while the liver is still able to perform its functions. As the scarring becomes more severe, the shape of the liver changes and it gets increasingly stiffer, reducing the blood flow and leading to a series of symptoms and complications. This is called decompensated cirrhosis, and it can become life-threatening without access to specialist health care.
Signs and symptoms of decompensated cirrhosis:
• Severe fatigue
• Loss of appetite
• Nausea
• Jaundice
• Weight loss
• Stomach pain
• Fluid retention
• Mental confusion
A person with decompensated cirrhosis should be in care with a liver specialist, routinely monitored for liver cancer and other serious problems, and be considered for a liver transplant.