
Over the past decade, transgender and gender non-binary (TGNB) individuals (i.e., people whose gender identity does not conform to their sex assigned at birth) have become more and more visible. There are currently about 1.4 million TGNB people living in the U.S. Unfortunately, many face discrimination in employment, education, housing, and healthcare as well as facing high rates of verbal, physical, and sexual violence. The HIV epidemic disproportionately affects the community, but awareness of prevention efforts using PrEP have been inadequate for this particularly vulnerable group.
Rates of HIV among TGNP people
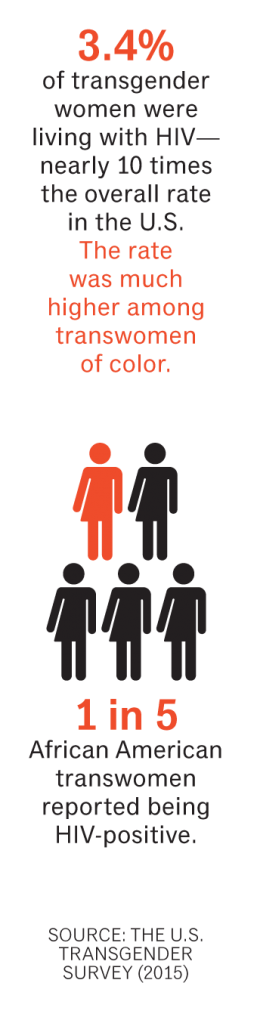
Though not uniformly collected, current data show that transgender women are disproportionately affected by HIV. A meta-analysis published in 2013 revealed that about one in four transgender women worldwide is living with HIV and they are almost 50 times more likely to be HIV-infected than the general population. The recent U.S. Transgender Survey (USTS) that studied over 28,000 TGNB people found that the rate of HIV infection among transgender women was 3.4%, which is nearly 10 times the overall rate in the country. The rate was much higher among transwomen of color. One in five African American transwomen (20%) reported being HIV-positive. Although rates were lower among transgender men and non-binary people (0.3% and 0.4%), there is an increased risk of infection among transgender men who have sex with cisgender (non-transgender) men.
PrEP research and TGNB people
In 2015 just over 39,000 people in the U.S. were diagnosed with HIV infection, a significant drop in new infections over the preceding decade. This decline is due to the success of public health programs that have promoted testing and early treatment of those who are newly diagnosed, but may also be due to the rollout of pre-exposure prophylaxis (PrEP). PrEP is a daily pill (brand name Truvada) approved by the FDA in 2012, containing two medicines (tenofovir DF and emtricitabine), that greatly reduces the risk of HIV infection. Despite the increased risk of HIV among transgender women, TGNB people are still not designated as a priority population for PrEP by the CDC, which prioritizes sexually active MSM, heterosexuals at substantial risk for HIV, and injection drug users.
The largest PrEP study, called iPrEx, enrolled about 2,500 HIV-negative gay men and transgender women from six countries. They took either a placebo (inactive pill) or Truvada. The study showed that the rate of HIV infection was reduced by 44% in people who were assigned to take Truvada. When people took their pills consistently they had even greater protection against HIV, over 92%.
A subanalysis that only looked at the 339 (14%) transgender women in the iPrEx study showed that there was no difference in the rates of new infections among those assigned to take Truvada and those assigned to take the placebo; i.e., the drug did not appear to be effective. Further investigations showed that transgender women who seroconverted while assigned to take Truvada had no evidence of the drug in their blood. The investigators concluded that adherence may be more difficult for transgender women who may be dealing with structural barriers to care and psychosocial issues, such as homelessness, depression, and substance use. It is also possible that women may prioritize other health issues, such as access to hormone care, over HIV prevention, especially if they are concerned that Truvada may affect the effectiveness of their hormones. It does appear that when taken consistently, Truvada is just as effective at preventing HIV infection among transgender women, since no infections occurred among those who had adequate drugs levels, equivalent to at least 4 tablets per week. Unfortunately we do not have good data about PrEP uptake or effectiveness among transgender men and non-binary people. Transgender men are often excluded from studies that enroll MSM, even if they have significant HIV risk factors.
Transgender people on PrEP
Before starting PrEP, people are screened for HIV infection, hepatitis B, and STIs and evaluated for kidney problems. While on PrEP, testing for HIV, STIs, and kidney function is usually repeated every 3 months. For transgender men who start PrEP, it is important to remember that they will also need to be regularly screened for pregnancy if they are having frontal (vaginal) sex with cisgender men, even if they are on testosterone, since this doesn’t completely protect against pregnancy. Other differences also exist for transgender men. Those who take testosterone will have an increase in muscle mass, which can elevate the serum creatinine. Since the creatinine level is used to evaluate kidney function, transgender men on testosterone should have their values interpreted using the usual male range of test results. Although PrEP is thought to reach adequate levels in rectal tissue after 7 days, it may take up to 20 days for maximum levels in vaginal tissue. Transmen who have vaginal sex will need to know that they may not be fully protected against HIV until they have been on PrEP for about 3 weeks.
Some TGNB people may have had gender-affirming surgeries, including genital reconstruction. For transgender women who have had vaginoplasty surgery, the vagina is usually created using scrotal and penile tissue. Although the skin is thought to be more resistant to infections than mucosal tissue, the neovagina does not naturally lubricate, and may be prone to small tears, ulcers, and abrasions, which may theoretically increase susceptibility to HIV and STIs. Transgender men may decide to have genital reconstruction to create a phallus (phalloplasty) or to extend the clitoris (metoidioplasty) and can choose to retain or remove the vagina, uterus and ovaries. It is important for providers to ask questions about surgeries and sexual behaviors in order to give appropriate information on HIV and STI risks, screening, and prevention. There is not a lot of information about the best ways to screen for STIs in those who have had genital surgeries, but the general rule is that testing should be based on the existing anatomy and the sexual behaviors that people engage in. We also do not have information about how these surgeries impact the tissue concentrations of PrEP drugs.
Truvada usually has few side effects, but nausea, vomiting, and headache can occur and generally resolve within four weeks. Some studies have also shown occasional changes in kidney function as well as small reductions in bone density. Bone issues may be a greater concern for transgender women who have higher rates of osteopenia and osteoporosis (low bone density), especially if they have had an orchiectomy (surgical removal of the testes). Ways to maintain bone health include not smoking, regular exercise, and maintaining a healthy diet. Transgender women who have had surgeries that include orchiectomy should be encouraged to continue hormones to reduce further bone loss.
Implementing PrEP
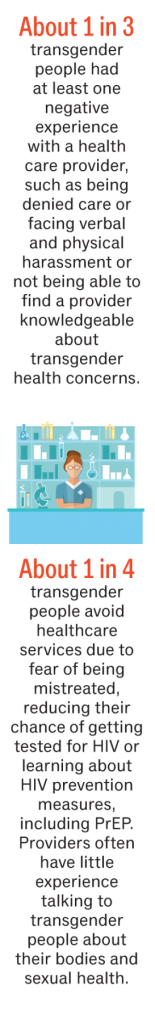
Even with the publicity following the iPrEx results, knowledge about PrEP remains low among communities at risk, especially among transgender people. In San Francisco a survey conducted in 2013 among transgender women showed that less than 14% had heard about PrEP. This occurred even though many of the women had risk factors for HIV infection, and would have benefited from using it. The lack of knowledge about PrEP is likely due to many things. Transgender people are often neglected in public health campaigns. Even more important is the fact that transgender people face many barriers when trying to access comprehensive primary care and sexual health services. The USTS showed that about 1 in 3 transgender people had at least one negative experience with a health care provider, such as being denied care or facing verbal and physical harassment or not being able to find a provider knowledgeable about transgender health concerns. These access issues are even worse for transgender people of color and those who have disabilities or who are sex workers. About a quarter of transgender people avoid healthcare services altogether due to fear of being mistreated, which lessens their chance of getting tested for HIV or learning about HIV prevention measures, including PrEP. Providers often have little experience talking to transgender people about their bodies and sexual health, and may not properly assess their risk factors for HIV and other STIs. They may also make assumptions, e.g., that transgender men are not at risk for HIV and fail to offer appropriate screening or HIV prevention.
Additional barriers
PrEP is expensive, costing about $1,200 a month as well as the added costs of testing and office visits. Cost can be a real barrier for transgender people, who may be unemployed or lack insurance, and who may be unaware that there are patient assistance programs to cover these costs. Difficulties also arise when TGNB people have identification or insurance cards with names or gender markers that do not match their gender presentation, including denial of medical care, verbal harassment, and physical assault. Name changes require a court order in many jurisdictions, which may be unaffordable for many. Transgender women might also worry that Truvada can negatively affect their hormones. The good news is that interactions are unlikely to happen between estrogens and the agents that make up PrEP.
Scaling up
PrEP is an extremely important addition to HIV prevention services, but is underutilized by TGNB people. There needs to be a realistic understanding of the barriers to its use in these communities and innovative approaches to improving access. Educational campaigns and materials need to be redesigned to ensure these are trans-inclusive, not only in words but in images that resonate with TGNB people. Future studies on PrEP implementation and trials evaluating new agents need to include TGNB people to ensure questions on efficacy, tissue concentrations, and drug-drug interactions are properly addressed.
Scaling up PrEP will require that health settings are safe and affirming of TGNB people, especially for those who may have had previous negative experiences. This includes allowing people to register under their preferred name, that staff ask about and use pronouns correctly and consistently, and that people are able to use public accommodation, such as restroom facilities, without harassment. Providers should improve their knowledge about transgender people, and ensure they are appropriately trained to conduct sexual health interviews that are respectful and affirming of trans-identities and that empower people to make informed decisions about risk and prevention.
Co-location of comprehensive sexual health services with transgender health services and hormone care is likely to increase PrEP uptake. Transgender people who have been mistreated in health settings and who avoid health facilities may be more comfortable accessing care in other settings, such as PrEP clinics housed within community-based organizations, implemented through pharmacies, or mobile medical units.
Addressing structural barriers to care through provision of legal services (e.g., assisting with name changes, housing, and employment discrimination), drug assistance programs for the under- and uninsured, wrap-around services to aid adherence, risk-reduction efforts, and programs that address mental health and substance use are all other important areas to consider.
Dr. Asa Radix is the Director of Research and Education and an infectious disease physician at the Callen-Lorde Community Health Center in New York City. Asa has 20 years experience working with transgender clients and is the clinical associate editor of Transgender Health.


