FDA approves Descovy for PrEP; Delstrigo and Pifeltro approved for switch treatment; Bictegravir, dolutegravir and Tybost for children; and more.

FDA approves Descovy for PrEP
As this issue went to press, the FDA approved the drug Descovy for use as PrEP (pre-exposure prophylaxis) in the prevention of sexually acquired HIV. However, the FDA did not approve Descovy PrEP for receptive vaginal sex, saying that its effectiveness had not been evaluated in this context.
The only other medication approved for HIV prevention, Truvada for PrEP, approved in 2012, does cover receptive vaginal sex.
Gilead Sciences, maker of Descovy and Truvada, entered into a post-marketing commitment (PMC) with the FDA to conduct a clinical trial evaluating the safety and efficacy of Descovy for PrEP in cisgender women and adolescent girls weighing at least 77 pounds (35 kg). The PMC will include a group taking Truvada for PrEP for comparison. Of note, some transgender men have a vagina and some use it for receptive sex with other men.
Descovy and Truvada are both HIV medications containing a pro-drug of tenofovir. Simply put, the pro-drug is converted into tenofovir (becomes active) after it enters the body. The pro-drug in Descovy is tenofovir alafenamide (or TAF) while the pro-drug in Truvada is tenofovir disoproxil fumarate (or TDF).
TAF and TDF are converted in different ways, and some research data indicate that TAF may not reach protective levels as high or as quickly in the vaginal tract as does TDF.
Descovy was studied as PrEP in gay men and transgender women. It was not studied in cisgender women. The most common side effect with Descovy PrEP was diarrhea.
Truvada is more than 92% effective in preventing sexually acquired HIV. Both Descovy and Truvada are taken as one pill once a day, whether used for HIV treatment or as PrEP.
See the FDA announcement at bit.ly/2OdwwQ2. Read more about Descovy, Truvada, and Truvada for PrEP in the Positively Aware HIV Drug Guide.
Follow avac.org and treatmentactiongroup.org for more information and advocacy updates. Treatment advocates have expressed concern over Descovy for PrEP, including preliminary indications that Descovy might be wrongly promoted as safer than Truvada.
Delstrigo, Pifeltro switch approved
The FDA has approved a switch indication for Delstrigo and Pifeltro.
Anyone with undetectable viral load of less than 50 on a stable HIV antiviral regimen can now switch to the single-tablet regimen Delstrigo or to a drug combination that includes Pifeltro. Individuals must be on a stable regimen for at least six months and have no drug resistance to doravirine (brand name Pifeltro, also found in Delstrigo) or to the other medications contained in Delstrigo, and no history of treatment failure.
Individuals could have previously been switched to a doravirine-containing medication using off-label prescribing. New Phase 3 data from the DRIVE-SHIFT clinical trial gave the FDA the evidence they needed to make a switch indication (usage) official in September.
Read more about Delstrigo and Pifeltro in the Positively Aware HIV Drug Guide.
Bictegravir and dolutegravir for children
In September, U.S. pediatric HIV treatment guidelines updated recommendations for therapy.
The single-tablet regimen Biktarvy (bictegravir/FTC/TAF) is now a preferred therapy for first-time treatment for adolescents aged 12 and older weighing at least 55 pounds (25 kg). Biktarvy is also an alternative regimen for initial use in children ages 6 and older weighing at least 55 pounds.
Tivicay (dolutegravir) plus two nucleoside reverse transcriptase inhibitors (NRTIs) is now an alternative regimen for first-time treatment for children aged three and up who weigh 44–55 pounds (20–25 kg). It was previously recommended for children weighing more than 55 pounds. Dolutegravir plus two NRTIs is found in the single-tablet regimen Triumeq. It is also found in Dovato and Juluca. Tivicay can also be taken separately with Descovy or Truvada.
For more information, go to aidsinfo.nih.gov and the Positively Aware HIV Drug Guide.
Harvoni for children
In September, the FDA approved the hepatitis C medication Harvoni for use by children 3–11 years old. (Harvoni was already approved for pediatric patients ages 12 and up.) Children must have:
- genotype 1, 4, 5, or 6 without cirrhosis or with compensated cirrhosis
- genotype 1 with decompensated cirrhosis, for use in combination with ribavirin
- genotype 1 or 4 and be liver transplant recipients without cirrhosis or with compensated cirrhosis, for use in combination with ribavirin
The weight-based dose is given once daily with or without food. Those with difficulty swallowing Harvoni tablets (available in different doses) can use the oral pellets formulation instead.
Harvoni is made up of two medications in one tablet, ledipasvir and sofosbuvir. The FDA also approved sofosbuvir by itself (brand name Sovaldi) for children 3 to 11, but this drug is only rarely used nowadays.
See the FDA announcement for treatment duration and more at bit.ly/2moWswc.
Tybost now for children
Tybost can now be used in children. Although not an HIV drug, Tybost is used as a “booster” to increase levels of the HIV medications Prezista and Reyataz.
- Cobicistat (Tybost’s generic name) and darunavir (the generic name of Prezista) are also in the single-tablet regimen Symtuza.
- There are also fixed-dose drugs with cobicistat in combination with Prezista or Reyataz (Prezcobix and Evotaz).
- Cobicistat is also in the single-tablet regimens (STRs) Stribild and Genvoya; these two medications have already been studied in children and approved for their use.
The FDA approved Tybost for pediatric use following new clinical trial data showing safety and efficacy in adolescents aged 12–17. Pediatric approval was made in October.
Children taking Tybost with Prezista must weigh at least 88 pounds (40 kg). Children taking Tybost with Reyataz must weigh at least 77 pounds (35 kg).
Read more about Tybost (and these other medications) in the Positively Aware HIV Drug Guide. See the FDA update at bit.ly/356Waf9.
The FDA approved Tybost for pediatric use following new clinical trial data showing safety and efficacy in adolescents aged 12–17. Pediatric approval was made in October.
Children taking Tybost with Prezista must weigh at least 88 pounds (40 kg). Children taking Tybost with Reyataz must weigh at least 77 pounds (35 kg).
Read more about Tybost (and these other medications) in the Positively Aware HIV Drug Guide. See the FDA update at bit.ly/356Waf9.
TB treatment update
Thanks to new findings in tuberculosis (TB) research, treatment updates for people also living with HIV were made in September.
The new research in TB diagnostics, therapeutics, pharmacology, and drug resistance led to changes in the U.S. HIV guidelines covering opportunistic infections (OIs) in adults and adolescents. Key highlights from the update announcement are below. Read more at aidsinfo.nih.gov.
- For people starting HIV therapy who are at high risk for developing TB-associated immune reconstitution inflammatory syndrome (TB-IRIS), preemptive prednisone is recommended as adjunctive therapy.
- The 3HP regimen (weekly isoniazid plus rifapentine for 3 months) for the treatment of latent tuberculosis infection (LTBI) is now recommended as an alternative regimen when provided as self-administered therapy or directly observed therapy (DOT).
- Four months of daily rifampin monotherapy is now recommended for the treatment of LTBI in patients who cannot receive isoniazid.
- When dolutegravir (Tivicay, also found in Juluca and Triumeq) is given with concurrent rifampin, it is recommended that the dolutegravir dose be increased to 50 mg twice daily. (Tivicay, which is normally taken as only 50 mg tablet once daily, would be taken twice a day. With Juluca or Triumeq, a 50 mg Tivicay tablet would be added to the daily regimen, ideally 12 hours apart from the Juluca or Triumeq dose.)
- Bictegravir (found in Biktarvy) is not recommended to be given with rifamycin-containing TB treatment.
- Isoniazid preventive therapy is not recommended for pregnant women until after delivery unless they are close contacts of a known patient with active TB disease.
- Prednisone is no longer recommended for the treatment of TB pericarditis.
- Isoniazid-monoresistant TB should be treated with 6 months of rifampin, pyrazinamide, ethambutol, and either levofloxacin or moxifloxacin.
Shingles vaccine update
U.S. HIV treatment guidelines in September updated the recommendations on using a vaccine against shingles in people age 50 or older. Healthy adults 50 years and older, including those living with HIV, should get two doses of Shingrix, separated by 2 to 6 months. You should get Shingrix even if in the past you had shingles, received Zostavax, or are not sure if you had chickenpox. There is no maximum age for getting Shingrix.
Shingles is a painful rash that usually shows up as a stripe around the torso, but can occur anywhere on the body. You cannot get a shingles infection from the Shingrix vaccine.
In addition, the guidelines say that:
- Shingrix is preferred over Zostavax.
- If Shingrix cannot be used because of allergy, intolerance, or unavailability, Zostavax can be taken as one subcutaneous dose (a shot under the skin). Zostavax should not be used by anyone with less than 200 T cells.
Shingles (herpes zoster) is caused by the varicella-zoster virus (VZV). VZV also causes chickenpox (varicella), usually in children and adolescents. VZV is not a sexually transmitted infection.
The section on ocular (eye) complications of VZV has also been expanded.
Shingrix is recombinant (inactive) zoster vaccine, or RZV. Zostavax is zoster vaccine live, or ZVL.
Due to a manufacturing problem, Shingrix is on back order; check with your pharmacy for availability.
Go to aidsinfo.nih.gov for more information.
8-week Mavyret in cirrhosis
Mavyret can now be taken for just eight weeks by individuals with compensated cirrhosis who are taking hepatitis C therapy for the first time (called “treatment-naïve”).
Previously, only treatment-naïve individuals without cirrhosis could use Mavyret for eight weeks. Those with compensated cirrhosis had to take it for 12 weeks.
The FDA approved the new treatment duration in October, reporting that, “Mavyret is now the first eight-week treatment approved for all treatment-naïve adult and pediatric patients ages 12 years and older or weighing at least 45 kg [99 pounds] with HCV genotypes 1–6 both without cirrhosis and with compensated cirrhosis.”
Twelve or 16 weeks of Mavyret must still be used by most individuals who had previously taken hep C therapy (called “treatment-experienced”).
Mavyret is a combination of glecaprevir and pibrentasvir.
The FDA added new data to the Mavyret label, as well as other information on topics such as liver function and drug interactions. Read the FDA update on its Mavyret changes at bit.ly/2nyFX1w.
OI updates: histoplasmosis
The U.S. guidelines on opportunistic infections (OIs) in people living with HIV were updated in September regarding histoplasmosis, a lung infection that is caused by fungal spores found in soil or in the droppings of bats and birds.
Medications taken to prevent histoplasmosis should not be discontinued by individuals on anti-HIV treatment until they have achieved at least six months of undetectable viral load with a T cell count greater than 250.
More information has been added on treating people who do not tolerate itraconazole, voriconazole, and posaconazole, which are used to prevent and to treat histoplasmosis. There is also additional discussion of data on measuring the Histoplasma antigen (a substance which shows that the person has been exposed).
Go to aidsinfo.nih.gov.
Crypto in children living with or exposed to HIV
U.S. pediatric HIV treatment guidelines in August updated the section on cryptosporidiosis (“crypto” for short). No major changes were made to the diagnosis and treatment of crypto in children living with HIV or those who were exposed to the virus in the womb. But minor changes were made to the information on epidemiology, clinical manifestations, and new diagnostic methodologies. There are also new resources listed for preventive measures. Go to aidsinfo.nih.gov.
U=U: The third U
In an essay for the British Medical Journal, Tamás Bereczky of the European AIDS Treatment Group (EATG) notes that the U=U (Undetectable equals Untransmittable) message is hugely important, but not so helpful for those lacking access to care. Read his reminder of a third “U”—universal access: bmj.com/content/366/bmj.l5554. Published in September, the essay includes suggestions to meet the need for diagnostics and antiviral drugs to promote the benefits of U=U, which means that people living with HIV who have undetectable viral load cannot transmit the virus to others.
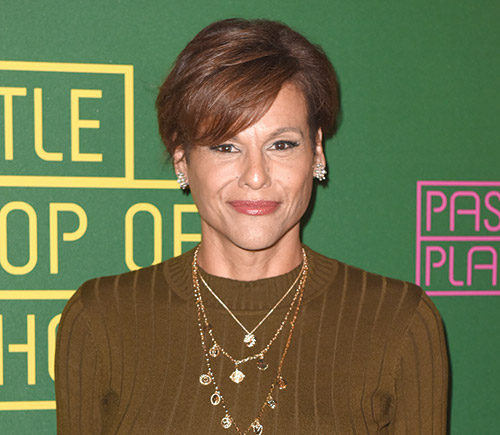
Alexandra Billings gets Wicked on Broadway
Alexandra Billings is set to join the Broadway show Wicked as Madame Morrible in January, becoming the first openly transgender actress in the role. A veteran performer with roots in Chicago, Billings is also openly living with HIV. She is probably most known for her role as Davina on the Amazon series Transparent. Her last Broadway appearance was in the 2018 comedy The Nap. Read her heartfelt interview with POSITIVELY AWARE editor Jeff Berry in the May+June 2017 issue: positivelyaware.com/articles/once-again-alexandra-billings.

In the clinic
There was one guy who came in, and after I spoke with him about PEP [post-exposure prophylaxis], he said very coldly, “I thought it was a pill.” Oh, did you think it was like a morning after pill? No, it’s two pills every day for one month. He didn’t want to do it. I talked with another guy for 20 minutes about PrEP [pre-exposure prophylaxis] and he was very interested. Then his HIV test result came back negative and he said, “Never mind.” Maybe what he was really interested in was PEP because he thought he might have been exposed to HIV over the weekend. We know that if you were exposed on Friday, you’re not going to test positive on Monday.
—Christopher Reynolds
Community Liaison, ASP Cares,
Las Vegas, speaking from the audience at a session on PEP at USCA 2019 in Washington, D.C. in September
Share your clinical and medical insights with Positively Aware for In the Clinic. Email e.vazquez@tpan.com.
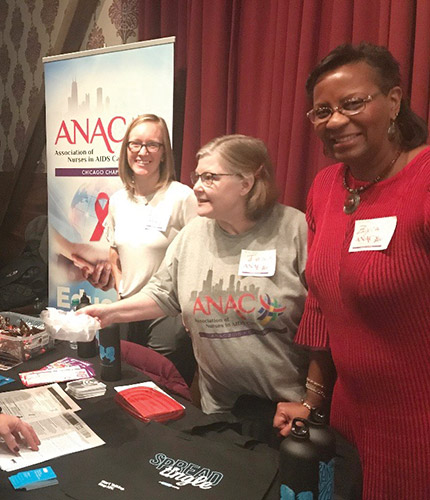
Chicago nurses mark 30 years of HIV care
Chicago Nurses in AIDS Care (CNAC) celebrates its 30th anniversary with a gala, Crimson and Pearls, on Saturday, December 7.
“CNAC is a wonderful organization for all people concerned with HIV to come together and share the depths of their experiences providing care and services to persons living with HIV,” said board president Zyra Gordon-Smith.
The association invites all HIV health and service providers, allies, and community members to join in celebrating its milestone anniversary.
Crimson and Pearls starts with cocktails at 6 p.m. and dinner at 7 p.m., followed by commemorative reflection and remembrances. And yes, there will be dancing.
Proceeds support CNAC’s mission to continue HIV education, advocacy, and health community networking through monthly programs and volunteer events. Additional proceeds will provide a nursing scholarship to attend the Assoication of Nurses in AIDS Care’s national conference. Tickets are $100, available through Eventbrite at bit.ly/2klNDT4.

Briefly Extras by Julie Taddeo
Second living kidney donation by PLWHIV
Karl Neumann had always considered becoming an organ donor. But the 52-year-old IT coordinator at Sentara Norfolk General Hospital in Virginia gave up hope when he was diagnosed with HIV 11 years ago.
The HIV Organ Policy Equity (HOPE) Act, passed in 2013, allows people living with HIV to donate their organs to recipients also living with HIV. As a result, Neumann has become the second successful kidney donor in the U.S. under the HOPE Act. (See “Where There’s HOPE” in the January+February issue to read about the first donor, Nina Martinez.)
The procedure took place at Duke Health, the only facility in North Carolina—and only one of five facilities in the U.S.—approved for HOPE Act transplants.
There have been more than 140 transplant procedures since 2014 involving organs from deceased donors who had HIV. According to the Organ Procurement and Transplantation Network, as of September 6, 2019 there were 220 people living with HIV who were in need of kidneys, and 16 were in need of a liver transplant.
It is a common and mistaken assumption that people living with HIV cannot be organ donors. Neumann hopes to end this misconception by bringing awareness to his story. If more people living with HIV become aware, they might decide to become donors themselves, increasing the viable options for patients awaiting transplants.
Register through Donate Life America at registerme.org. Look for HOPE in Action studies at clinicaltrials.gov. Go to hopkinsmedicine.org/transplant/living_donors. Email mailto:hopeinaction@jhmi.edu.

Jonathan Van Ness gives HIV stigma a makeover
Jonathan Van Ness, 32, hairdresser, television persona from Netflix’s Queer Eye, and author of his recently released memoir, “Over the Top: A Raw Journey to Self Love,” has added HIV activist to his lengthy resume. The Quincy, Illinois native has overcome a difficult past of sexual abuse, drug use, sex addiction, and depression to become who he is today.
In a recent op-ed in The New York Times, author and sociologist Celeste Watkins-Hayes of Northwestern University points out that Van Ness’ story exposes a larger issue she has observed within her research on women living with HIV: the correlation between victims of sexual abuse and HIV. Hayes points out that assault victims do not typically acquire HIV from the incidents, but rather are more likely to engage in riskier sexual behavior later on in life. She explains how it can destroy one’s perception of self and regard for safety. Van Ness’ memoir recognizes and promotes the importance of love and self-acceptance. The story is “not going to be pretty,” he explains, “but it’s my truth and if I don’t share it I won’t be able to help others.”
Since coming out, Van Ness has released a promotional video advocating for Planned Parenthood by encouraging people to get tested for STIs. Motivated to support the organization where he went to get tested seven years ago, he also highlights the importance of Title X, the federal grant program dedicated to providing accessible healthcare and regular STI screening. As a proud “member of the beautiful HIV-positive community,” he hopes to combat stigma through education.
Van Ness was undetectable within two weeks after his diagnosis and starting treatment; he takes one pill a day, and continues to live an extraordinary life. He wants people to understand HIV is not what it used to be considered in the past; it is no longer a terminal illness, but a chronic manageable condition.
New effort targets HIV care disparities in the South
The Merck Foundation has launched a $7 million, five-year initiative aimed at improving access to care and health outcomes of people living with HIV in underserved and vulnerable communities in the southeastern U.S.
HIV Care Connect will be implemented in three sites: Care Resource in Miami, Florida; Medical Advocacy and Outreach in Montgomery, Alabama; and the University of Mississippi Medical Center in Jackson, Mississippi. Each location will receive a grant intended to link community-based programs and promote long-term engagement in HIV care. The program will also encourage private and public partnerships to combat socially determined barriers of health.
The developers hope the initiative will identify plausible practices for improving access to HIV care. Learn more about the program at msdresponsibility.com/access-to-health/key-initiatives/hiv-care-connect.

Rugby's Gareth Thomas comes out--again
Having come out as gay in 2009, retired British rugby legend Gareth Thomas disclosed in September that he is living with HIV. He said he made the announcement to get in front of media reports that were being used to blackmail him or force him to disclose.
Thomas, 45, experienced depression and thoughts of suicide; he did not want the public to be aware of his status. He initially thought that suicide would be “the easier way out,” but has come to realize the importance of confronting his fears. He said that keeping the secret had been taking a toll on his wellbeing.
Thomas has since chosen to be transparent about living with HIV and said he will focus his efforts on HIV awareness and education to overcome stigma. It’s important for someone living with HIV to have a strong support system, he said. He added that although he may be vulnerable, he is not weak.
HIV and heavy drinking
A new study released by Boston University School of Medicine (BUSM) shows a correlation between individuals with untreated HIV who drink heavily (three or more drinks a day for women; four or more a day for men) and harmful immune activity. The study examined three biomarkers which correspond to key immune functions: systemic inflammation (inflammation throughout the body), monocyte activation (fever response), and altered coagulation (blood clotting). Research indicates that raised levels of these responses are associated with an increased risk of death.
There were 350 participants, 71% of whom were male and the average age was 34. The study participants had little risk of chronic inflammatory diseases (diabetes, obesity, or kidney disease) associated with aging. The study relied on self-reported alcohol use (collected at three points over two years), along with a blood-based marker called PEth (phosphatidylethanol).
Elevated levels of all three biomarkers were found in individuals with HIV who reported heavy drinking and had higher levels of PEth. It is important to note, however, that the results were observational and the relationship between systemic inflammation and monocyte activation were not linear. The researchers said further research is needed to verify causality. The study was published in PloS One at bit.ly/2m9UgZh.
New initiative for transgender community
Gilead recently established the TRANScend Community Impact Fund to improve the lives of transgender individuals, who acquire HIV at three times the national average.
In 2017, the company pledged $100 million over 10 years to reduce HIV stigma and address inequalities in the U.S. South, and in 2018 awarded $17 million in grants that helped fund programs for people living and aging with HIV.
The TRANScend initiative originated from an advisory panel made up of transgender people and leaders of organizations that provide services to people of trans experience. They stressed that they face multiple challenges including spousal abuse, stigma, and inadequate access to healthcare. Because many of these challenges intersect, it is hoped that the grants will help with more than just HIV-related issues.
Gilead has pledged $2 million for the initiative and is currently accepting applications from community groups across the U.S. -Julie Taddeo


